Canadian Panel Member Guide to Immigration Medical Examinations 2020
- An introduction to the immigration medical examination process
- Section 1: general guide for panel members
- Your work as a panel member
- Becoming a panel member
- Getting your unique identifier and login
- eMedical user identification
- Panel member designation is not permanent
- A summary of your responsibilities
- Using eMedical
- Performance guidelines and expected timelines
- If you are not available for IME activities
- Using a locum tenens
- Referring applicants to consultants and specialists
- If you relocate your practice
- Ethical conduct and conflicts of interest
- Administrative instructions
- Quality assurance, incidents and complaints
- The immigration medical examination
- General information about the IME
- How do I determine what examinations are required?
- Verifying an applicant’s identity and preventing fraud
- Required documents
- If an applicant does not have approved identification
- If you have an identity concern
- Client Declaration and Notice
- Medical Report – Client Biodata and Summary (IMM 1017)
- Upfront Medical Report – Client Biodata and Summary (IMM 1017B UPFRONT)
- Medical Report (501 Medical examination)
- Resettlement Needs Assessment (Exam 948 in eMedical)
- Pregnant Client – X-Ray Deferred (IMM 5733)
- Additional forms for the IME
- Additional information for submitting IME forms
- Panel members who work in Canada
- The interim federal health program (IFHP)
- Your work as a panel member
- Section 2: supplementary information
- Instructions for completing paper-based IMES
- General information about the IME
- How do I determine what examinations are required?
- Verifying an applicant’s identity
- If you have an identity concern
- Required documents
- If an applicant does not have approved identification
- Client Declaration and Notice
- Medical Report: Client Biodata and Summary (IMM 1017)
- Excessive demand exempt (EDE) applicants
- Non-EDE applicants
- Refugee overseas applicants
- Upfront Medical – Client Biodata and Summary (IMM 1017B upfront)
- Medical Report (IMM 5419)
- Resettlement Needs Assessment (IMM 5544)
- Pregnant Client – X-Ray Deferred (IMM 5733)
- Additional Forms for paper-based IMEs
- Additional information for submitting forms
- Legislation related to the immigration medical examination
- The Immigration and Refugee Protection Act
- The Privacy Act
- The Access to Information Act
- Acronyms, initialisms and definitions
- Instructions for completing paper-based IMES
- Section 3: appendices
- Appendix I: How to contact us
- Appendix II: Client Declaration and Notice (IMM 5743)
- Appendix III: Forms
- IMM 1017: Medical Report – Client Biodata and Summary
- IMM 1017B UPFRONT: Upfront Medical Report – Client Biodata and Summary
- IMM 5419 Medical Report
- IMM 5725: Activities of Daily Living (ADL)
- IMM 5728: Acknowledgment of HIV Post-Testing Counselling
- IMM 5733: Instructions for Pregnant Client - X-Ray Deferred
- IMM 5734: Specialist’s Referral Form
- IMM 5738: Chart of Early Childhood Development (CECD)
- Appendix IV: List of immigration medical examination technical instructions
- A) TIs related to process changes resulting from eMedical implementation
- B) TIs related to conditions of significance
- Cancer or malignancy
- Cognitive impairment in adults
- Diabetes, hypertension, chronic renal or cardiac diseases
- Debilitating conditions
- Breast, genital, gynecological and rectal examinations
- Developmental delay in children
- Hearing impairment or deafness
- Hepatitis/liver disease
- HIV
- Psychiatric conditions
- Syphilis
- Tuberculosis
- Appendix V: Training
An introduction to the immigration medical examination process
A program administered by IRCC
Immigration, Refugees, and Citizenship Canada’s (IRCC) Migration Health Branch administers and delivers Canada’s medical screening program for people who want to visit or immigrate to Canada.
If someone applies to stay in Canada, they need to meet a set of criteria, including medical standards for admissibility. To be considered admissible, an applicant must not create a danger to public health or public safety, and must not create excessive demand on Canada’s healthcare or social services.
A network of panel members and regional offices
IRCC relies on a network of panel members – physicians and radiologists – to conduct immigration medical examinations (IMEs) on people applying to live here.
Panel members practising in Canada and overseas work with one of four IRCC regional medical offices to report the medical findings of the IMEs they carry out. Our offices are located in Ottawa, Canada; London, UK; Manila, Philippines; and New Delhi, India.
Who needs an IME?
Many criteria go into the decision about whether someone coming to Canada needs an IME, including how long they plan to stay, their type of visa application and where they have lived or travelled. In most situations, visa and migration officers determine who requires an IME before the applicant sees a panel physician.
Some people applying to stay in Canada will contact your clinic to get an appointment for an upfront medical exam. Others have files already created electronically, which you will use as the basis for performing an IME.
If you have questions about which category applies to an applicant, contact your Regional Medical Office (RMO).
What this guide tells you
This guide provides comprehensive information for panel members, including:
- details about completing your application to become a panel member
- the general responsibilities of your work, including your ethical and professional responsibilities
- how to conduct an IME, including how you determine what examinations to do, the forms you will need, and how to administrate the paperwork
- how to use the Interim Federal Health Program (medical insurance)
- legislation that applies to conducting IMEs
Leveraging eMedical
IRCC has implemented an electronic, web-based processing system called eMedical for performing and reporting on IMEs.
eMedical is an information technology project among Canada, Australia, New Zealand and the USA that saves processing time, improves the integrity of the examination program, and provides many other benefits. Panel members working in countries where eMedical is implemented must use it to complete and transmit all IMEs.
A small number of panel members do not have access to eMedical. Those who work with a paper-based system will find key information about how to conduct an IME in Part 2 of this guide.
Check back for new information
The process for medically screening immigrants, and the immigration process itself, are subject to change. IRCC will update this guide as needed, and the updates will override the text they replace. This means the online version of the panel member guide is guaranteed to be the most current. Your RMO will also send you new information as it becomes available.
Please consult our list of acronyms, initialisms and definitions for clarification as you read this guide.
Visit IRCC’s website for more information on Canada’s immigration program.
Section 1: General guide for panel members
Your work as a panel member
Becoming a panel member
Thank you for considering becoming a panel member. If you are reading this section of the guide, you have likely been contacted by IRCC about participating in the immigration medical examination (IME) system and you’re looking for additional information about the application process.
If this is the case, to conduct IMEs on behalf of IRCC, ensure that you have submitted the following:
- a series of forms that IRCC has provided:
- application form
- consent to share information
- consent to use eMedical where available
- acknowledgment of having read this guide
- acceptance of designation
- all required documents, such as proof of professional license and certification
- IRCC’s orientation about the IME process, which includes reading and understanding this guide and participating in discussions with IRCC Migration Health Branch personnel
- all steps of IRCC’s IME training, including eMedical training, either individually or through a group activity
Panel members are not authorized to perform IMEs for IRCC during the orientation phase.
Getting your unique identifier and login
Once IRCC has received all your forms and documents, your regional medical office (RMO) will review your application and, if your status is approved, send you a unique identifier number (P number). Your P number enables IRCC to perform quality assessments of your work.
The unique identifier starts with the letter “P” followed by eight or more digits (e.g. P12345678). Your unique identifier will be embedded electronically in each IME or chest x-ray you submit through eMedical. (Paper-based clinics, please see our special set of instructions.)
Your unique identifier should be included in all your correspondence with IRCC.
eMedical user identification
All eMedical users will have a unique login ID and password to access the system. The eMedical login information is linked electronically to your unique identifier.
You must not share your eMedical login ID with any other person or let anyone else use it to submit IMEs or chest x-rays. It is the responsibility of the panel physician and panel radiologist to ensure all of the material entered into eMedical is accurate before submitting the IME. (Paper-based clinics, please see our special set of instructions.)
Panel member designation is not permanent
IRCC’s migration officials and medical officers regularly consult each other on how many panel members are needed in a given location. When you are designated as a panel member, you do not have permanent status, and completing the designation process does not create a contractual relationship with IRCC. This has several implications:
- IRCC does not guarantee that any panel physician will receive a specific number of cases per year.
- IRCC increases or reduces the number of panel members in a given location according to its needs.
- As a panel member, you are expected to stay in good standing with your licensing body and notify IRCC about any investigation into your license or your authority to practice medicine.
- You can be terminated as a panel member following a complaint or dispute about your performance. Please find more information about meeting IRCC’s performance standards and evaluations, and the complaints and resolution process.
- You can also be terminated if you do not reply or provide documents such as applicants’ medical files when IRCC requests.
- Your designation may be terminated at any time on 30 days’ notice. Your status may also be suspended at any time to allow for an investigation.
A summary of your responsibilities
Panel members are authorized to perform IMEs, arrange for diagnostics and investigations, and complete IME forms. You do not have the authority to assess or determine whether the medical conditions of applicants are grounds for health admissibility to Canada. More specifically, you may not give applicants an opinion on their medical admissibility. That decision rests with Canadian migration officers.
Panel members performing IMEs should ensure that they meet IRCC’s performance service standards and that there are no conflicts of interest in providing services. You are also required to help prevent fraud and abuse of Canada’s immigration laws, submit to performance evaluations, follow proper procedures for absences, and use English or French in your communications with IRCC.
For all applicants, the Canadian IME will include an examination by a panel member and a medical assessment by IRCC. Sometimes, applicants can be asked to undergo further medical evaluation to ensure compliance with Canada’s Immigration and Refugee Protection Regulations.
The assessment of whether or not a client is admissible on health grounds is largely based on findings reported in the IME, but it can include information unknown to panel members.
In parallel to the Immigration Medical Examination process, panel members are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, panel members are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Here are your general responsibilities, organized according to your role in the IME process.
All panel members
As a panel member, you must do the following:
- Stay familiar with the latest version of this guide and all associated administrative and IME instructions.
- Follow instructions about verifying the applicant’s identity.
- Hold valid professional registration and licensing issued by local or national regulatory authorities and ensure your RMO has a copy, along with an official translation in either English or French, if it is not in one of Canada’s official languages.
- Maintain valid professional registration and licensing throughout the relationship with IRCC. If your license or other certification expires, it is your responsibility to send updated documents to your RMO promptly. If you fail to do so, you could be removed from the Panel Network.
- Keep all immigration medical information in your possession confidential and store it securely.
- Ensure that the fees you charge for immigration medical services fairly represent the services you perform, and that they comply with local guidelines or those of a medical association or group.
- Ensure that a list of fees and charges for the IME and related expenses is either posted in your clinic, office or website, or emailed to applicants before their examination:
- The list should include fees for required radiological and laboratory investigations, postage or courier charges, and other services.
- Any special fees for groups or large families should also be listed.
- Copies should be available for applicants on request.
- All applicants should receive a receipt for services.
- Ensure that all panel clinic staff members who you supervise are aware of the requirements and standards for the IME and its procedures, and that they understand your role and obligations.
- Always offer to have a chaperone present for an IME. If a chaperone is declined, this should be documented.
- Ensure that individual and clinic contact information is up to date. eMedical users must keep their contact information updated in the system and also alert their RMO when they make changes. Those who use paper-based forms must inform their RMO of changes in contact information.
- Ensure high-quality work by all professionals involved in conducting IMEs, including staff members and specialist consultants.
Panel physicians
As a panel physician you must do the following:
- Get the applicant to complete the IRCC’s Client Declaration and Notice Form, which explains how the information collected during the IME will be used and stored.
- In addition to filling out the Client Declaration and Notice form, you are required to follow your country’s guidelines and legal requirements for documenting client consent for medical exams and tests, including vaccination.
- Follow your country’s public health regulations for notifying authorities when you identify a condition that may present a public health concern, such as active tuberculosis (TB), untreated syphilis, human immunodeficiency virus (HIV) or acute viral hepatitis.
- Conduct a complete, age-appropriate IME. Depending on an applicant’s age, and according to IRCC’s technical instructions (TIs), the IME can include physical and mental examinations, routine tests and appropriate pre- and post-test counselling for applicants who undergo HIV testing. You will find links for each TI in Appendix IV.
- Coordinate all the IME results and the IME report to be submitted to the RMO, including lab results and chest x-rays, as well as reports from other consultants and specialists when required by your RMO.
- Inform your RMO as soon as possible when you suspect fraud, misrepresentation or non-compliance.
- Ensure that the laboratory you use:
- is aware of the requirements and standards for the Canadian IME
- is registered and licensed by a local or national regulatory authority and can provide proof of that when the RMO requests it
- has appropriate quality control procedures in place
- follows instructions for verifying the applicant’s identity
- complies with administrative requirements
- completes the Laboratory Requisition and Report section of the Medical Report (IMM 5419) accurately
- prevents fraudulent substitution
Chief radiologists
As a chief radiologist, you must do the following:
- Monitor the performance of all nominated radiologists and their staff, and work with IRCC to resolve cases or issues of concern related to nominated radiologists. (A nominated radiologist is a licensed radiologist nominated by the chief radiologist to perform, grade and submit chest x-rays for Canada’s IMEs.)
- Ensure that every nominated radiologist undertaking Canadian immigration radiological examinations is qualified as a specialist in radiology, that their license is valid, and that they are registered to work in the country where they practice.
- Provide your RMO with the names, dates of birth, genders and unique email addresses of each of your nominated radiologists.
- Add your nominated radiologists to the clinic profile in eMedical and notify IRCC of these changes so that we can grant them access to submit Canadian cases.
- Supervise all nominated radiologists – including ensuring accuracy and quality control of the Chest X-Ray Requisition section of the Medical Report (IMM 5419).
- Ensure that all nominated radiologists complete IRCC’s training regime.
- Ensure that radiological examinations are conducted at the agreed site(s).
- Implement and monitor the procedures for checking the identity of applicants.
- Circulate any communications from RMOs and IRCC to nominated radiologists and their staff.
- Advise IRCC of any anticipated interruption of service and any change related to the list of nominated radiologists. This includes absences, changes to staff, clinic contact details, capabilities and other working arrangements that could affect service.
- Ensure that nominated radiologists conduct chest x-rays (routine posterior-anterior view for applicants 11 years old and older) according to the instructions laid out in this guide – and that they adhere to all procedures in this guide.
- Ensure the quality and integrity of the IME process as it relates to radiology.
Nominated radiologists
Nominated radiologists are panel members who have been nominated by the chief radiologist at their clinic to help conduct IMEs. Your chief will have verified that you are a specialist in radiology, that your license is valid and that you are registered to work in the country where you practice. Your personal information will have been transmitted to your RMO to obtain a unique identifier, or “P” number for you to use.
As a nominated radiologist, you are responsible for managing your caseload and submitting chest x-rays for IMEs in a timely manner.
Chief and nominated radiologists
Both of these groups must do the following:
- Conduct chest x-rays (routine posterior-anterior view only for applicants 11 years old and older) according to the instructions laid out in this guide.
- Ensure that the associated panel physician is informed without delay of all chest x-rays where there is a high suspicion of active pulmonary tuberculosis.
- Follow all procedures laid out in this guide.
Using eMedical
eMedical is a web-based system used by IRCC for electronically recording and transmitting IMEs. eMedical is also used by the Australian Department of Home Affairs, Immigration New Zealand, and the United States Centers for Disease Control and Prevention. It is available around the globe with a few exceptions; therefore, all panel members must submit IME results via eMedical whenever possible.
In rare cases where a panel member is unable to use eMedical (no internet signal, no computer available due to crisis, etc.), your RMO will consider allowing you to submit paper-based IME results. (Paper-based clinics, please see our special set of instructions.)
Where eMedical is available, all panel members must:
- complete and submit all IMEs and related documents through the eMedical system
- maintain and keep a secure eMedical account, including user ID, password, and secret questions and answers, that you do not share with anyone in your clinic
- ensure all clinic staff who enter data into eMedical have their own account information
- ensure that your personal and business information in the system is updated and accurate at all times
- notify your RMO immediately if your password becomes known by an unauthorized person
- take all reasonable steps to guarantee the security of applicants’ personal information in eMedical
- ensure that applicants’ personal information contained in eMedical is treated in a manner consistent with Canadian privacy laws – including, but not limited to, protecting collected information against loss and unauthorized access, use, modification, disclosure and other misuse
- ensure all panel clinic staff under your supervision are aware of and abide by the requirements and standards for completing IMEs in the eMedical system
Performance guidelines and expected timelines
Here are IRCC’s service standards for IME activities. Panel physicians are expected to perform 80 percent of these activities within the timelines set out in the table below. If you are unable to meet these standards, you must notify your RMO. You may be asked to provide a justification for the delay. If you are unable to schedule an appointment with a client within 20 days, you must provide them with proof that an appointment has been scheduled. These standards also apply when you are providing information after the initial IME results were submitted.
| Activities | Time frame (in calendar days) |
|---|---|
| Appointment with panel physician, including upfront medicals | 10 days |
| Appointment with panel physician in cases where the applicant is furthered | 10 days |
| Obtain lab results | 7 days after date of the exam |
| Obtain x-ray results | 7 days after date of the exam |
| Submission of the IME to RMO by the panel physician | 10 days of date of the exam |
| Responding to correspondence from RMO | 48 hours |
| Forwarding inactive immigration medical files to the RMO | Paper-based: 8 week old IMEs eMedical users: Files are auto deleted after 365 days of inactivity |
| Notifying the responsible RMO of any change in practice location or contact information | At least 14 days before the change takes place |
| Notifying the responsible RMO of any absence of 7 days or more | At least 14 days’ notice, (preferably by email) |
| Being available for provision of performance and technical information related to the IME process (e.g. quality assurance visits, annual audits) | 7 days’ notice |
If you are not available for IME activities
If you plan to be unavailable for IMEs for more than seven calendar days, you must inform your RMO. Here are the rules that apply to your absences:
- Enter leave dates directly into your eMedical profile.
- If possible, tell your RMO when you will depart from work and when you will return. This is important information for applicants to know.
- If a locum tenens will replace you while you are away, tell your RMO at least 14 days in advance, preferably by email. This will enable your RMO to approve your recommended replacement and activate their eMedical account. For more information, see our section below on using a locum tenens.
- If you are identified as “on leave” in eMedical, you cannot submit IMEs. Your locum tenens can complete IMEs on your behalf.
- If you have extended or repeated unreported absences, your status as a panel member may be revoked.
Please note that you are required to keep your contact information updated in the system.
Using a locum tenens
As panel member, you may ask your RMO to approve a locum tenens for your clinic if:
- you will be absent from your clinic for longer than seven days
- your clinic is experiencing a high volume of requests for IMEs and does not have the capacity to meet IRCC’s service guidelines
Here is the process for requesting a locum tenens:
- Contact your RMO to get approval. (Your RMO can consider your request before you send documentation.)
- Send your RMO the name and contact information for the locum tenens you want, as well as a copy of the locum’s medical registration and licence.
- Send your RMO a statement from your proposed locum saying that they have read this guide and agree with the standards and requirements it defines. Note that before you recommend a particular physician or radiologist as your locum tenens, you must be satisfied that they have the qualifications and experience to perform IMEs, and that they understand the reporting procedures and are aware of any updates issued by eMedical or IRCC’s Migration Health Branch.
-
If your RMO approves the request, it will send you a written response by letter or email. You can then tell your locum that they have been authorized.
You must give your RMO at least 14 days’ notice, preferably by email, for every period of time where the locum will be acting on your behalf, or where a locum is required to temporarily increase capacity in the clinic. This gives the RMO time to activate the locum’s eMedical account. You also need to specify an end date for the locum.
- IRCC will provide your locum tenens with a unique identifier.
- The locum will get their own password for eMedical. You must not share your password with the locum.
- The system will be updated with appropriate information about your locum, and their eMedical account will have a specific end date that aligns with the dates approved by your RMO.
- If you are terminated by IRCC, this will automatically cancel prior approvals for your locums.
Referring applicants to consultants and specialists
Panel physicians must not refer clients to specialists unless instructed by the Regional Medical Office, with exceptions for referral of cases of suspected active TB and HIV specialist consultations. All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME if obtainable at the time of IME submission.
Panel physicians must not refer clients to specialists for IME purposes unless instructed by the Regional Medical Office, with exception of referral of cases of suspected active TB for specialist consultations.
All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME if obtainable at the time of
If you relocate your practice
If you become a panel member and relocate your practice, you must tell your RMO because your designation is related to where you work. If you relocate, you may lose your designation as a panel physician. Once IRCC has assessed its requirements in your new location, it will let you know whether it needs you as a panel member there. You will have an opportunity to respond.
As a panel member, you must ensure IRCC has up-to-date documentation throughout the relationship. If your license or other certification expires, you must send the updated documents to IRCC. If you fail to do so you could be removed from the IME network.
Ethical conduct and conflicts of interest
As a panel member, you are expected always to conduct yourself ethically. When you conduct an IME for an applicant, you must carry out your professional obligations with competence, integrity and loyalty – the same way you do with all your patients.
You must also ensure that the people you employ and associate with in your practice meet these requirements. In conducting IMEs, you must:
- be courteous and respectful towards all applicants
- be mindful of applicants’ time, dignity, privacy and cultural practices
- display integrity in professional practice, particularly in relation to conflicts of interest
Here are some of the more specific ways in which you are expected to behave:
- Do not behave in a manner where you appear to be acting in a biased way because of a personal interest. You are expected to show professional behaviour and perform your IME-related activities in keeping with the principles of proper ethical medical practice and IRCC policy.
- Provide appropriate and timely advice to an applicant when you discover a significant medical concern they either did not know about or did not fully understand. In such a situation, you must inform the applicant of the concern and, with their consent, refer them to an appropriate clinician.
- Perform the duties of your practice impartially, uninfluenced by fear or favour.
- Avoid situations where your private, financial or other interests might reasonably be thought to conflict with conducting IMEs for applicants.
- An example where a conflict of interest could arise is if there is a working relationship between your clinic and an immigration consulting firm, where you accept their referrals to conduct IMEs and, in return, you refer your clients to them.
If the following issues or events arise, you must notify your RMO as soon as possible:
- You are suspended or come under investigation by your medical regulatory authority.
- You learn that you have been accused of malpractice or improper behaviour, even if it has not yet been investigated.
- You discover inappropriate activity relative to the provision of IMEs by your clinic, office, laboratory, or radiology centre staff.
- You become aware that any associated panel member is under investigation for a criminal activity or has been charged with or convicted of a criminal offence.
IRCC reserves the right to suspend a panel member’s designation after an investigation has been completed by a medical or regulatory authority.
The Code of Conduct for Panel Members
The Canadian Government has close ties with its Migration 5 (M5) intergovernmental partners, namely the United Kingdom, New Zealand, Australia and the United States of America, as part of the M5 Health Working Group (M5HWG) in the area of migration health. The M5HWG share a collective desire to support panel members, aiming to ensure consistent and reliable, high-quality IME related services are performed, as well as to ensure the high standards of the behaviour of panel members and the level of service provided to individuals undergoing an IME are being met and maintained. Therefore, the M5WHG members have developed the Code of Conduct for Panel Members to articulate the required standards of behaviour and conduct of panel members and define protocols and procedures if there is a breach of the Code.
The Code of Conduct for Panel Members is accessible through the eMedical Support tab, under Support Material.
It is essential that all panel members are aware of, and comply with the Code. Panel members who breach the Code may be subject to action at the discretion of the relevant Migration 5 country.
Equal rights for all applicants
The principle of equal rights applies to all applicants that a panel member encounters, regardless of their:
- race, national or ethnic origin, colour, religion
- gender or sexual orientation
- age, mental or physical disability
Canada protects the rights and privacy of an individual to identify in the gender of their choice and express their gender and sexual orientation freely. As a panel member, you are required to show the same respect and privacy for IRCC applicants.
This includes using proper gender pronouns and preferred names when addressing an applicant. Outside of IME procedures, you should never disclose an applicant’s medical information, including gender expression and sexual orientation.
Accommodating cultural and other needs
Some applicants may ask for special accommodation during the IME due to personal or cultural sensitivities. As good practice, you should routinely offer to have a chaperone present when you are examining a client. Patient consent is always necessary for a chaperone to be present.
Female applicants may be uncomfortable with a male examiner (and vice versa), in which case you should either offer to have a chaperone present during the examination or make alternate arrangements that preserve the integrity of the IME.
Preferably, the chaperone should be a trained health professional familiar with the examination so they can confirm it was appropriately conducted. If that is not possible, you can use non-medical staff. In some cases, it may be reasonable for you to suggest that the patient choose a person to bring to the examination.
Overall, you should accommodate personal and cultural sensitivities, while keeping in mind that IME standards must be respected. When you make an accommodation, record on the examination form the type of accommodation you provided and the roles other people played who may have been present during the IME.
Should you not be comfortable examining a client for any reason – due to a conflict of interest, dispute, religious reason, personal belief, etc. – it is your responsibility to tell the applicant and your RMO.
Using Canada’s official languages
English and French are the official languages of Canada and, as a panel member, you must be able to communicate verbally and in writing in at least one of them. You must also complete the IME in one of the official languages. Other things to keep in mind:
- Inform IRCC of your preferred official language for correspondence, as well as any other language you speak. You can tell us about your other languages in a drop-down list in your eMedical profile.
- You must choose your preferred official language for processing IMEs in eMedical.
- When you submit reports from specialists as part of an IME, you must do so in one of Canada’s official languages. If a specialist submits a report in another language, you must have it translated.
Employing a medical interpreter
When you perform an IME, you may find yourself examining an applicant who does not speak one of Canada’s official languages – or any language you speak. In these cases, you and your clients would benefit from the services of an interpreter.
You may consider obtaining the service of a professional interpreter for clients, particularly in regions where a high proportion of clients may need a translator. An interpreter could also be a friend, a relative of the applicant or any other person. The person acting as an interpreter:
- should be at least 18 years old (the interpreter must be mature enough to understand and appreciate the importance of the proceedings and questions)
- must have sufficient knowledge of English or French
- must be able to provide the required assistance
While providing this service is not an obligation, it is highly recommended by IRCC in order to provide accessible IME services to clients.
Administrative instructions
IRCC’s Migration Health Branch has put together this list of administrative instructions to guide you in various situations – from how to advertise your services to how to handle complaints from applicants.
Guidelines for managing records
All the forms, documents and results of investigations involved in completing IMEs are the property of IRCC once the IME is submitted. You can access the IME for 365 days after you submit it.
Panel members who perform IME-related activities must follow the procedures and guidelines here for copies and files as well as for original documents and information:
- Keep a paper or electronic copy of the original IME for at least two years – or for the minimum retention time for medical documents in your area of jurisdiction, whichever is longer.
Information you collect during the IME is for Canadian immigration medical purposes only. You may not use it for other purposes – including research, clinical studies or investigations – without IRCC’s consent. Direct your consent requests to the Integrated Medical processing network by:
Email: IRCC.MHBIMPN-RITDMDGMS.IRCC@cic.gc.ca
Mail:
Senior Director, Integrated Medical Processing Network
Migration Health Branch
Immigration, Refugees, and Citizenship Canada
250 Tremblay Road
Ottawa, ON K1G 5P4- Forward original documents and information related to an IME to your RMO electronically via eMedical.
- Save a full copy or a summary of the IME for your own records.
- Print a copy of the IME by clicking the “Print health Case” button at the bottom of the Health Case details window.
- Print out a full copy or a summary of the IME to give to the applicants or, in the case of children, their guardian – unless there is a strong reason to not do so. Examples include when there is information in the IME from a different client, or when releasing the information could reasonably lead to another person or entity being subject to significant inappropriate behaviour by the applicant.
- Applicants may request a copy or a summary of their IME at any time. You should provide the requested information as long as your office has retained it – unless there is a strong reason to not do so.
- Applicants who wish to have further access to IRCC’s review and assessment of their IME can do so by filing an access request.
Advertising your services
You may wish to advertise your IME services outside your clinic by using a website, or electronic or printed material. If you do this, the following rules apply:
- You may:
- include information about regular fees associated with an IME (including user and related fees), the services included in your fees, your clinic’s address and contact information
- provide links to Government of Canada websites
- You may not:
- post a summary of this information, as it changes frequently
- associate a Canadian flag with your website or advertisement
- use IRCC’s insignia in any way
- use the eMedical insignia or logo in any way.
How to communicate and where to send your questions
Regional medical offices
You will have regular contact with your RMO about medical and non-medical issues. Regional medical offices are your point of contact for all business issues, questions and comments about immigration medical cases and examinations, and about the immigration medical program. Your RMO will also update you on IME processes from time to time.
Questions and information about specific cases should always include identification details, such as the IME, unique medical identifier number (UMI) or unique client identifier number (UCI). To protect applicants’ confidentiality and personal information, information requests should not identify them by name or include their date of birth.
eMedical systems support
If you have questions about eMedical (regarding user functionality, adding or removing users, submitting exams, etc.) you can:
- consult the eMedical support material under System User Guides and Quick Reference Guides
- send the question via the email box that your RMO reserves for panel physician questions
For all other inquiries related to eMedical – issues with system glitches, unscheduled outages, etc. – contact the eMedical systems support team.
Canadian government officials and third parties
The Privacy Act says that you should never provide information about a specific case over the phone, private email or other means if you cannot verify the identity of the other person. Even acknowledging that you have a file on a specific applicant can constitute a breach of their privacy. If you have any doubts, consult with your RMO.
The media
The media may become interested in the IME of a particular individual and contact you for information. You must never provide the media with information about a particular case – or any confidential information about the immigration system or an applicant.
Refer all requests for comment or information to your RMO.
Remember that, as a third-party physician, you are doing IMEs on behalf of the Government of Canada. This means that all IMEs and their contents belong to the Government of Canada and not to you. Never grant a request from a third party – including a lawyer – for a copy of an IME. Instead, direct parties making requests like these to the Government of Canada’s online service for access to information or personal information.
Applicants
Applicants may have questions about the immigration process, particularly when RMO officials ask for additional medical information or investigations.
Although you can explain what the requested information means from a general medical point of view, you are not authorized to explain or justify any immigration reason for these requests. You should simply explain that the request came from the RMO, that you are only a contact person between RMO and the applicant, and that the applicant can contact their migration office for more information.
Specific questions about the IME process could include the following:
- the time it takes IRCC to complete the medical assessment process
- the time it takes between completion of the IME and the next steps of the immigration process or the issuing of a visa
- administrative or policy aspects of the program
- other immigration-related issues, including why the applicant’s IME is not linked to their application
Applicants can find many answers to their questions by reading IRCC’s website or by using IRCC’s help centre. These tools include the phone numbers applicants can use to contact the IRCC help line, and the forms to submit web enquiries about immigration applications. Some applicants can also use their ‘myCIC’ web account to ask questions.
You should never direct applicants in the following ways:
- Never send applicants to your RMO or share any RMO or RMO staff contact details with applicants or their representatives. RMOs will not have all the information they need to reply to most types of enquiries and will be unable to verify the applicant’s identity.
- Never direct clients to the eMedical help desk.
Ensure that your staff is aware of these instructions.
Charging and collecting fees for IMEs
All applicants, except those eligible for the Interim federal Health Program, are responsible for paying all fees and costs associated with their IME. These fees include the following:
- panel physician services
- radiological and laboratory services
- consultations with specialists
- investigations and treatment – e.g. when referred for treatment of tuberculosis or syphilis
- costs related to sending medical documents to the RMO
You may also charge reasonable fees for:
- follow-up visits in the case of furtherances
- providing copies of the IME to the client upon request
- missed appointments in accordance with local standards of practice
- user fees – e.g. the IME clinic is in a hospital and the hospital charges the client a fee for using the facility
Rules associated with charging fees:
- All current user or additional fees must be included in the cost of your clinic’s IME wherever the cost is displayed or advertised.
- You should charge reasonable fees and either post a fees list in your clinic, office or website, or email your fees to the applicant before their examination.
- Applicants should receive an itemized receipt that clearly indicates the services for which you charged them and includes the applicant’s name, age and IME number.
- Your fees must reflect local conditions and service charges. Consequently, the fees for IMEs may vary from country to country and even within a country.
Quality assurance, incidents and complaints
Clear and transparent procedures for quality assurance, responding to complaints and resolving problems improve IRCC’s service to applicants and the overall integrity of the immigration medical program.
Our quality assurance regime
IRCC’s Migration Health Branch conducts regular quality assurance and quality control exercises, and its officers will occasionally visit panel members to ensure they are meeting IRCC’s IME performance guidelines.
When your RMO asks, you should make yourself and your staff available for evaluation, monitoring, training, quality assurance, training activities and onsite visits. Your RMO will usually give you seven days’ notice. Migration officers may also conduct administrative visits to panel sites on the behalf of the RMO.
When an RMO requests, you must provide, in a timely fashion, all the forms and documents they have asked to review (e.g. panel member appointment forms, quality assurance activities). The procedure for completing the IME is spelled out in this guide and your performance in this regard will also be evaluated.
Your RMO will evaluate all complaints and incidents related to your performance conducting IMEs.
If an incident occurs during the IME process
If you have a disagreement with an applicant during an IME, or confusion arises or an event occurs that might compromise client service, you should report the incident to your RMO, providing full details. Here are some examples of incidents you should report:
- The applicant becomes upset, angry, threatening or violent toward you or your staff.
- The applicant claims that you are deliberately delaying the IME process or requesting unnecessary investigations for personal gain.
- The applicant refuses to undergo parts of the examination or investigation.
- You or your clinic staff become aware of attempts by the applicant to falsify certain aspects of the IME, or clinical or laboratory investigations.
- You or your clinic staff are asked to overlook or alter some aspects of the IME, or of clinical or laboratory investigations.
- The applicant threatens to complain about the IME service or the IME process itself.
- You feel that reporting an unusual situation may be instructive to the program or provide useful information to other panel members should they encounter a similar situation.
Email your respective RMO regarding the situation. Reports to your RMO should include:
- the date of the incident
- the client’s IME, UMI or UCI number
- a brief description of the incident
What happens when someone complains about you?
Complaints are common in any client service procedure. Applicants, the people representing them and other people outside IRCC may make complaints about the IME and its related services. IRCC personnel may also make critical comments or notify RMOs about errors, performance issues, or other situations of concern regarding the IME and the services panel members provide.
If someone makes a complaint against you or your clinic, you may receive a letter of concern from your RMO. If this happens, you must comply with the instructions and timeframes indicated in the letter, including replying by the date that your RMO indicates. If you expect your reply to take longer, you should notify your RMO.
IRCC’s Migration Health Branch will carefully consider your opinions and viewpoints – as well as those of the person making the complaint – when they review a complaint or concern.
Resolution process for complaints and performance issues
If you engage in misconduct or poor performance, you may lose your designation as a panel member. Here are some examples of situations where you or your clinic staff are performing poorly:
- Unacceptable behaviour or demonstrated misconduct:
- unprofessional or unethical conduct or activities
- breaching client confidentiality
- illegal activities
- performing IMEs after any loss or suspension of medical license
- reports or indications of physical, verbal or sexual abuse by panel members or their staff
- Continued failure to maintain an acceptable level of performance as set out in this guide or in written instructions from the RMO. This includes when a panel member continues to be deficient, after they are repeatedly notified, in the following areas:
- timely and correct completion of IMEs
- appropriately providing necessary laboratory and clinical investigations and activities
- gathering and managing medical information
- transferring information to IRCC’s Migration Health Branch in a timely manner
- following the instructions in this guide
Resolving issues
Your RMO will address minor incidents or performance deficiencies by sending you a letter outlining the steps you must take to correct the issue. This could include additional training.
For serious or repeated administrative or clinical issues – such as harassment, allegations of sexual misconduct or illegal activities – the RMO can suspend you, issue a letter summarizing the facts that gave rise to the complaint and provide you with an opportunity to reply.
While your panel member designation is suspended, you must stop all IME activities related to taking on new applicants. Your RMO will tell you how you should work with applicants you are already seeing.
If you are suspended, your RMO will conduct an assessment once it has received your reply. If your response is deemed satisfactory, your RMO will inform you of its decision and potentially reinstate you with appropriate recommendations. Alternatively, your designation could be permanently terminated.
If you are terminated
IRCC has complete authority over the management of the panel member network. The number of panel members that we require may change if demand for IMEs shrinks in your area. If you are terminated for operational reasons, your RMO will notify you in writing at least 30 days in advance.
However, if your designation is terminated because of performance deficiencies or complaints, the termination is effective on the date of your RMO’s notification letter.
If you retire or wish to resign
Panel members may retire or ask to be removed from the panel network at any time. Send written notification to your RMO, including the date you expect your activities will end.
The Immigration Medical Examination
This section provides panel members who use eMedical with information they need to complete IME and associated forms.
Panel members using a paper-based system should refer to our supplementary section in this guide. IRCC has redesigned IME paper forms to ensure they are consistent with eMedical IMEs.
General information about the IME
The IME consists of a medical history, physical examination, age-specific laboratory tests and age-specific chest x-ray.
Usually, routine, age-specific laboratory and radiologic tests include:
- urinalysis – applicants age 5 and older
- chest x-ray (posterior-anterior view) – applicants age 11 and older
- syphilis – applicants age 15 and older
- HIV – applicants age 15 and older
- serum creatinine – applicants age 15 and older
A medical examination includes any or all of the following:
- physical examination
- mental examination
- review of past medical history
- laboratory test
- diagnostic test
- medical assessment of records respecting the applicant
- urinalysis – applicants age 5 and older
- chest x-ray (posterior-anterior view) – applicants age 11 and older
- syphilis – applicants age 15 and older
- HIV – applicants age 15 and older
A medical examination does not include breast, genital, gynecological or rectal examination. If there is a history or a clinical suspicion of malignancy, record any relevant information in the medical history portion of the IME.
Panel members may request additional lab tests for an applicant younger than the recommended age based on an applicant’s individual risk factors.
It also be necessary to screen applicants below the ages indicated. See IRCC's technical instructions for more information.
How do I determine what examinations are required?
eMedical provides a questionnaire for all applicants. Depending on their answers, eMedical may populate the form with additional questions and possibly instruct you to send the applicant for consultation with a specialist.
As the panel physician, you are never required to decide on a course of treatment or additional tests. Once you submit the applicant’s IME, a medical officer working with your RMO will decide if additional tests are required and notify you through eMedical. Alternatively, instructions may be provided by your RMO before eMedical prompts have been updated. Instructions from your RMO supersede any prompts from eMedical.
Verifying an applicant’s identity and preventing fraud
It is essential that you identify applicants throughout the IME process to ensure the person undergoing the IME is the same person applying for entry to Canada, and that there is no substitution at any time during the lifecycle of the IME. An applicant’s identity is confirmed through a process of verifying the applicant’s photographs and identity documents.
- You must take a live digital photograph of the client in your clinic and upload it to eMedical.
- Photographs must meet IRCC’s photographic specifications standards (PDF, 506 KB).
- The eMedical system will include the photograph on all requisitions and referrals (laboratory, radiology, specialists and others).
Required documents
The applicant must submit a passport or other identification document acceptable for the Canadian IME. IRCC strongly prefers that applicants submit passports. This includes new passports and passports expired for no more than a year.
Other approved identification documents include the following:
- national ID card (an original birth certificate is an acceptable national ID document for applicants under the age of consent only)
- driver’s licence (Drivers licenses will be accepted as valid identification only if issued by Canada, the United States, Australia, New Zealand and the United Kingdom and presented in panel clinics located within the same country.)
- refugee travel document
- Red Cross travel document
- UN laissez-passer
- Seaman’s book
- Organization of American States travel document
- Refugee Protection Claimant Document
If an applicant does not have approved identification
If an applicant does not provide an approved identification document, they must provide an alternative form of identification. You should not turn such applicants away, and you should conduct the IME as long as the applicant presents some form of identification.
If the applicant provides identification that is not approved, you must report “identity concern” in the eMedical system.
Important: To ensure the integrity of the IME process, the applicant must use the same identity document for all components of the IME, including laboratory, radiology and specialist referrals. Please inform applicants accordingly.
If you have an identity concern
If you cannot confirm that the person who has arrived for an IME is the person on the ID documents being presented, you should report that as an ID concern. In all cases except upfront medicals, biodata and information extracted from the applicant’s visa application will already appear in eMedical. You should compare this information with what the client attending the IME is presenting.
You should not report as an ID concern any minor differences in the eMedical information and the ID document such as misspelling of names, minor errors in date of birth or differences in validity dates.
If the applicant provides personal details that seem inconsistent with the information on the identity documents they submit, you must identify the concern in the eMedical system. For paper-based IMEs, report your concern on the IMM 1017: Medical Report – Client Biodata and Summary form.
Scan the identity document you are concerned about and attach a copy to the health case in the IME. You should then complete the IME according to customary procedures. The document will be submitted to IRCC once you have completed the IME.
IRCC will investigate your concern about the applicant’s identity.
Client Declaration and Notice
(See our sample Client Declaration and Notice form in Appendix II.)
Before undergoing an IME, all applicants must complete the Client Declaration and Notice form. A legal guardian or parent may provide and sign the declaration on behalf of the applicant if the applicant is under 16 years of age or is unable to complete and sign the declaration for reasons of incompetency (for example, if they have reduced mental capacity).
The Client Declaration and Notice form includes the following:
- a declaration stating that all information provided at the time of the IME is true and complete
- a notice stating that the IME information will be collected and temporarily stored in the eMedical system on segregated databases located in Australia
- a notice explaining that the collection, use and disclosure to IRCC of IME information follows Canada’s Immigration and Refugee Protection Act or protects the health and safety of Canadians
- a notice explaining the collection, storage, use and disclosure of vaccination information where the applicant has consented to the disclosure of this information to IRCC
Other important details:
- eMedical will automatically enter the applicant’s information on the Client Declaration and Notice form beforehand.
- You should print the form from eMedical and provide it to the applicant. The applicant must sign the copy of the Client Declaration and Notice provided in eMedical. Forms that have been altered or translated into another language are not acceptable.
- You or your staff should review the Client Declaration and Notice form with the applicant and answer any questions.
- The Client Declaration and Notice form is not a consent document and should not be construed as consent for the purpose of the IME or for vaccination.
- You must ensure to obtain client consent according to your country’s guidelines or legal requirements before performing medical tests and procedures required for the IME and before administering any vaccination, where applicable.
- You must ensure that the applicant understands and accepts that any relevant personal information collected during the IME process, including IME information and any vaccine-related information, when applicable, will be disclosed to IRCC.
- If an applicant does not complete the Client Declaration and Notice form, you cannot carry out the IME and you must notify your RMO.
- The applicant (or legal guardian/parent) must sign and date the Client Declaration and Notice form.
- You must scan and upload the form to eMedical.
- Tick the Client declaration check box in eMedical.
- You cannot submit the IME information in eMedical unless the Client Declaration and Notice form is attached.
Medical Report – Client Biodata and Summary (IMM 1017)
(See our sample IMM 1017 form in Appendix III.)
IRCC has implemented one standard form, the Medical Report – Client Biodata and Summary (IMM 1017), for all immigration categories. This form displays information such as:
- client information (biodata)
- immigration information
- IMM type: excessive demand exempt (EDE), non-EDE, or refugee overseas (see below for an explanation)
- IME grading
- panel physician declaration
Excessive demand exempt (EDE) applicants
EDE applicants are people who cannot be deemed inadmissible on the grounds that they would place an excessive demand on publicly funded Canadian health and social services. EDE applicants include refugees, refugee claimants, individuals with protected person status, and certain clients in the family classes.
However, EDE clients are assessed for:
- danger to public health
- danger to public safety
Non-EDE applicants
Non-EDE applicants are assessed for:
- danger to public health
- danger to public safety
- excessive demand on publicly funded Canadian health and social services
Refugee overseas applicants
Refugee overseas applicants are automatically assessed as EDE. Panel physicians must complete and submit the Resettlement Needs Assessment Form (IMM 5544) for overseas refugees.
IRCC typically issues the Medical Report – Client Biodata and Summary (IMM 1017) form with the applicant’s information and immigration information sections completed.
Applicants who have been issued a Medical Report – Client Biodata and Summary (IMM 1017) must present the form to your clinic when they arrive for their IMEs. The form will include two applicant identifiers: IME number and UCI number. (Note: This form may not include a client photo).
- Clinic staff must search for the applicant’s health case in eMedical using the IME number. They may search using the applicant’s name and passport number, or UCI number or UMI number.
- Clinic staff should confirm the applicant’s identity by comparing the applicant’s information with the approved identity document.
- The clinic must take a digital photo of the applicant and upload it to eMedical to verify the applicant’s identity throughout the IME process.
- The panel members involved in the applicant’s IME then complete all components of the examination in the eMedical system.
Upfront Medical Report – Client Biodata and Summary (IMM 1017B upfront)
(See our sample IMM 1017B upfront form in Appendix III.)
An upfront medical is an IME performed when an applicant reports to a panel physician with no paper Medical Report – Client Biodata and Summary (IMM 1017) or file in the eMedical system. Upfront medical examinations are generally permitted for students, visitors and workers who are applying to be temporary residents of Canada.
Only certain applicants are permitted to undergo an upfront medical. When it is not possible to confirm whether an applicant is permitted an upfront medical, you should perform one and indicate that the applicant is a “worker”. Please note that all members of an application should be identified under the same category. Therefore, if the principal applicant (say, the mother) is a worker, all children on the application should also be identified as workers.
These exams do not apply to family members being sponsored by a permanent resident of Canada. Whenever IRCC makes changes to the rules about individuals who can undergo an upfront medical, panel physicians are notified by their RMO.
Here is the procedure for doing upfront medical exams:
- You must first search eMedical for the applicant using their name and identity document number (e.g. passport number) to confirm that they do not already exist in the system. Always perform this step.
- If the applicant does not exist in eMedical, click “create case.”
- Enter the applicant’s personal details:
- title
- family name
- gender
- date of birth
- country of birth
- Enter the identity document details. Clinic staff will check the applicant’s identity with the approved identification document. (Note: a live photo of the applicant must be taken and uploaded to eMedical at a later step during the IME.)
- Enter the applicant’s preferred language.
- In the “Proposed Visa Application Details” section, select the appropriate upfront category from the drop-down list (student, worker, visitor or family EDE).
- Click “Create.”
- Proceed to upload and attach the applicant’s photograph.
- Complete “Identity Confirmation”.
- An “Information Sheet” letter will be generated by the system and must be printed and given to the client for submission to IRCC along with the visa application.
Panel physicians must ensure that they provide the applicant with proof that they have completed their upfront medical examination. For eMedical, the proof is the “Information Sheet” letter that gets printed. Applicants must include this proof when they submit their visa application.
If the applicant has received instructions for further examinations, you do not need to repeat or submit a new IME; you should simply remind the applicant to provide the migration office with proof of the upfront medical examination.
Since an IME is valid for 12 months, you should remind applicants to submit their visa application along with proof that they have completed their upfront medical examination well before the expiration date; otherwise, the client may have to undergo a second IME.
Medical Report (501 Medical examination)
You will use the applicant’s medical report to assess their medical condition. The medical report may be completed by clinic staff or the applicant, but you as the panel physician must review it to confirm the information.
Medical conditions that do not impact the immigration medical assessment
The following medical conditions do not impact the immigration medical assessment. If noted during the exam, check the medical history of the affected organ or system as normal and report your findings in the general comments section. Assign these cases an A grading if there are no other significant conditions.
- hypothyroidism or hyperthyroidism
- any history related to pregnancy, childbirth and gynaecology (such as C-sections, gestational diabetes or hypertension, IUDs or other birth control, fibroids, non-cancer hysterectomy)
- history of illness, injuries and surgeries with current normal function (such as repaired ventricular septal defect [VSD] or atrial septal defect [ASD], orthopedic injuries, appendectomy, negative biopsies or scopes, hepatitis A)
- asthma and allergies
- skin conditions not currently requiring treatment with biologic medications (such as psoriasis, acne, vitiligo, striae, uticaria)
- stable musculoskeletal conditions with no or minimum impact on function (such as scoliosis, history of fractures, osteoarthritis, joint replacement)
- cosmetic and plastic surgery not related to a disease process (such as bariatric surgery, breast implants, rhinoplasty, keloid removal, digit amputation)
- dental observations (such as caries, dentures)
- obesity
- professional tattoos and piercings
Medical history questions
You must provide details along with all “Yes” answers to medical history questions. IRCC requires the following information:
- date of diagnosis
- date of treatment or surgery
- relevant medications
- current status of the condition (and, if applicable, the prognosis)
You must either provide this information in the comments section or attach a report to the IME.
The following table lists additional requirements when the answers to medical report questions show abnormality – whether the IME is completed in eMedical or on paper. See IRCC's technical instructions for more information.
Table: Medical history questions
| Question | Related TI | IMM type | Requirements if “yes” in eMedical |
|---|---|---|---|
| Tuberculosis (TB), treatment for tuberculosis | Tuberculosis TI | EDE and non-EDE clients | Lateral CXR & AP CXR if ‹11 years old, Chest x-ray examination |
| Close household or work contact with tuberculosis (within last 5 years) | Tuberculosis TI | EDE and non-EDE clients | IGRA or TST, lateral CXR & AP CXR if ‹11 years old, Chest x-ray examination |
| Prolonged medical treatment and/or repeated hospitalization for any reason, including a major operation or mental illness | N/A | EDE and non-EDE clients | Medical report, if available when IME is submitted or if RMO requests |
| Psychological/psychiatric disorder (including major depression, bipolar disorder or schizophrenia) | Psychiatric conditions TI | Obtain x-ray results | Report from psychiatrist, psychologist or treating physician (attach all existing results and reports from labs and previous specialists) |
| History of HIV | HIV TI | EDE and non-EDE clients | HIV, CXR, Hepatitis B and C, syphilis, IGRA or TST regardless of age, and HIV specialist report including CD4 count, HIV viral load, and when antiretroviral medications will be needed |
| An abnormal hepatitis B or C blood test | Hepatitis / Liver disease TI | EDE and non-EDE clients | HIV, CXR, Hepatitis B and C, syphilis, regardless of age |
| Cancer or malignancy in the last five years | Cancer or Malignancy TI | non-EDE clients | Oncology report |
| Diabetes | Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Screen for signs or symptoms and presence of end-organ damage. |
| Heart condition including coronary disease, hypertension, valve or congenital disease | Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Screen for signs or symptoms (including blood pressure) and presence of end-organ damage. Serum creatinine, regardless of age |
| Blood condition (including thalassemia) | N/A | non-EDE clients | Check for history of admission. |
| Kidney or bladder disease | Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Urinalysis, serum creatinine (eGFR if abnormal); regardless of age |
| An ongoing physical or intellectual disability affecting current or future ability to function independently or be able to work full-time (including autism or developmental delay) | Psychiatric conditions TI and Cognitive impairment in adults TI | EDE and non-EDE clients | Activities of daily living (ADL) if > 5 years old, Chart of Early Childhood Development (CECD) if < 5 years old, consult TI for complete requirements |
| Addiction to drugs or alcohol | Psychiatric conditions TI | EDE and non-EDE clients | Only if the RMO requests – a psychiatrist’s, psychologist’s or treating physician’s report that specifically comments on previous threatening behaviour and if there is evidence of IV drug use, HIV, hepatitis B and C, regardless of age. The report must also specifically address if it is reasonably likely the client will exhibit future behaviour that might be a threat to the client or others. |
| Prescribed pills or medication (excluding oral contraceptives, over- the-counter medication and/or natural supplements) | N/A | EDE and non-EDE clients | List relevant medications and mention the indication |
| For female clients: a) Are you pregnant? |
N/A | EDE and non-EDE clients | N/A |
| b) If yes, what is the expected date of delivery? | N/A | N/A | eMedical generates this Pregnancy Deferral Letter. |
| c) If yes, do you wish to defer your chest x-ray at this time? | N/A | N/A | N/A |
Physical examination
As the panel physician, you must complete the physical examination. You must provide details of all abnormal findings during the physical examination. IRCC requires the following information:
- history
- diagnosis
- treatment details (including dates and medications)
- lab results
- specialist reports (as required)
- current status
- prognosis
You may enter this information in the comments section or attach a report to the IME in eMedical.
The following table lists additional requirements when the answers to physical examination questions show abnormality. See IRCC's technical instructions for more information.
Table: Physical examination
| Physical examination | Related TI | IMM type | Requirements if abnormal |
|---|---|---|---|
| Was a chaperone offered? | All TIs | EDE and non-EDE clients | Not applicable. Offer a chaperone to everyone. If a chaperone is declined, this should be documented. |
| Ear/nose/throat/mouth | N/A | EDE and non-EDE clients | N/A |
| Hearing | Hearing impairment or deafness TI | EDE and non-EDE clients | N/A |
| Eyes (including fundoscopy) | N/A | EDE and non-EDE clients | N/A |
| Best distance visual acuity (with or without correction) | N/A | EDE and non-EDE clients | N/A |
Blood pressure (clients = 15 years of age)
Normal readings
|
Diabetes, hypertension, chronic renal or cardiac diseases TI | EDE and non-EDE clients | Repeat blood pressure |
Repeated blood pressure (clients = 15 years of age)
Normal readings
|
Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Screen for signs or symptoms (including blood pressure) and presence of end-organ damage serum creatinine regardless of age |
| Cardiovascular system | Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Serum creatinine, regardless of age, |
| Respiratory system | Tuberculosis TI | EDE and non-EDE clients | If signs of TB: CXR, HIV, regardless of age |
| Nervous system: sequelae of stroke or cerebral palsy, other neurological disabilities | Debilitating conditions, Activities of daily living, and/or Developmental milestones: Chart of early childhood development TIs | EDE and non-EDE clients | Complete Activities of daily living, Development milestone: Chart of early childhood development and/or an assessment of cognitive functioning forms |
| Mental and cognitive state | Cognitive impairment, Activities of daily living, and/or Developmental milestones: Chart of early childhood development TIs | EDE and non-EDE clients | ADL if > 5 years old, CECD if < 5 years old, consult TI for complete requirements |
| Intellectual ability | Cognitive impairment, Activities of daily living, and/or Developmental milestones: Chart of early childhood development TIs | EDE and non-EDE clients | ADL if > 5 years old, CECD if < 5 years old, consult TI for complete requirements |
| Developmental milestones (clients = 5 years of age) | Developmental milestones: Chart of early childhood development TI | EDE and non-EDE clients | Complete Developmental milestones: Chart of early childhood development form |
| Gastrointestinal system | Hepatitis/liver disease TI | EDE and non-EDE clients | N/A |
| Musculoskeletal system | Debilitating conditions TI and Activities of daily living TI | EDE and non-EDE clients | Complete activities of daily living if > 5 years old, CECD if < 5 years old |
| Skin and lymph nodes | Cancer and HIV TI | EDE and non-EDE clients | Screen for skin cancer, leprosy, surgical scars, tattoos and piercings. Inspect/palpate neck, axilla and groin for lymphadenopathy |
| Evidence of substance abuse (e.g. venous puncture marks) | Psychiatric conditions TI | EDE and non-EDE clients | Complete psychiatrist’s report and, if evidence of IV drug use HIV, hepatitis B and C screening, regardless of age |
| Endocrine system (such as evidence of complications from diabetes) | Diabetes, hypertension, chronic renal and cardiac diseases TI | non-EDE clients | If diabetes is present, proceed with screening. |
| Are there any physical or mental conditions that may prevent this person from attending a mainstream school, obtaining full-time employment or living independently now or in the future? | Psychiatric conditions and Cognitive impairment TI | EDE and non-EDE clients | ADL if > 5 years old, CECD if < 5 years old, consult TI for complete requirements |
Laboratory Requisition and Report
eMedical will generate laboratory requisitions with applicant biodata and a photograph already printed on them. The system will also generate mandatory tests according to the applicant’s age and clinical findings.
Staff must document any identity concerns in eMedical. In such cases, laboratory testing may continue, and the panel physician will report the concerns to IRCC for follow up.
Urinalysis
A urinalysis is mandatory for all clients five years of age or older.
PPs and their clinic staff must NOT directly observe the collection of urine samples. Should there be a concern that a client has provided a falsified sample, the PP should grade the IME B and enter their concerns as a comment.
Refer to the Diabetes, hypertension, chronic renal or cardiac diseases TI for detailed recommendations on screening.
Syphilis serology
Syphilis is significantly prevalent in many regions of the world. You must pay special attention during the IME for all clients that have risk factors for syphilis, particularly those originating from areas with a high prevalence of syphilis.
Syphilis screening is required for all clients 15 years of age and older undergoing an IME. You must also request syphilis testing for clients below the age of 15 with any of the following risk factors:
- signs or symptoms compatible with syphilis infection
- high-risk sexual activity (for example, unprotected anal or vaginal sex, or multiple sexual partners)
- history of another sexually transmitted infection such as HIV, herpes, chlamydia, gonorrhea
- history of being born to a mother diagnosed with syphilis
- history of sexual contact with a known case of syphilis
- history of pregnancy
- for men, a history of having sex with other men
- history of sex work
- injection drug use
The evaluation consists of a medical history, physical examination and laboratory tests. You are required to report:
- if the applicant shows any signs or symptoms related to syphilis
- if the applicant has had a previous syphilis diagnosis
- evidence of recent or previous treatment
Symptoms are non-specific and it is entirely possible to go through the early stages of the infection without knowing about it.
See IRCC's technical instructions for more information – in particular, the syphilis TI.
If you see positive syphilis serology results from an applicant, you must:
- treat the syphilis according to the Canadian Guidelines on Sexually Transmitted Infections and provide proof of treatment
- accept previous treatment carried out according to the Canadian Guidelines on Sexually Transmitted Infections and provide proof of such treatment
IRCC requires the following treatment information:
- dates
- medications
- dosages
To prove that treatment has been provided to the applicant, you may either include proof of treatment information in the general supporting comments of the syphilis test section or attach a report to the IME in eMedical.
HIV serology
HIV screening is required for all clients 15 years of age or older undergoing an IME. Panel physicians must also request HIV screening for clients below the age of 15 with any of the following risk factors (TB high-risk group, refer to TB TI):
- signs and/or symptoms compatible with HIV diagnosis
- history of being sexually active
- history of another sexually transmitted infection such as syphilis, herpes, chlamydia, gonorrhea
- history of sharing contaminated needles, syringes and other infected equipment and drug solutions for injection drug use
- history of receiving unsafe injections, blood product transfusions or medical procedures that involve unsterile cutting or piercing
- accidental needle stick injuries, including among health workers
- suspected active tuberculosis, hepatitis B, hepatitis C
- tattoos, body piercing, or acupuncture not thought to be done with aseptic technique
- history of being born to an HIV positive mother
- any child showing failure to thrive
You should also do the following:
- Provide the applicant with culturally sensitive, age and gender appropriate pre- and post-test counselling.
- Consider legal, ethical, social and human rights issues.
- If you use an interpreter, select one who is unbiased and has no connection to the applicant. Family members or friends cannot act as interpreters. The applicant must pay the cost of a professional interpreter.
- Provide pre-test counselling that includes information on the following:
- how HIV is transmitted and prevented
- a description of the testing procedure
- confidential HIV testing, reporting and record handling
- the meaning of HIV screening test results, including the possibility of false positive or false negative results
- the need to inform anyone at risk of infection if the test is positive
- the applicant’s consent to undergo testing
You can find detailed information about how to manage pre- and post-test counselling in International Organization for Migration (IOM) Guide for HIV Counsellors: IOM HIV Counselling in the Context of Migration Health Assessment.
For all clients with positive HIV testing, panel physicians must provide a completed (signed and dated) IMM 5728: Acknowledgement of Post-test Counselling form, available in Appendix III.
Chest X-Ray Requisition and Report
Routine posterior-anterior chest x-rays (CXRs) are mandatory for applicants 11 years of age or older. If a chest x-ray is required for a child less than 11 years old, an anteroposterior view is mandatory. A panel physician should request a CXR, regardless of age, if the medical questionnaire reveals a history of tuberculosis infection or treatment in applicants or their close contacts. All chest X-rays must be submitted in DICOM format. DICOM tag elements must state the client’s name, DOB, gender and the institution name.
The CXR must be examined for:
- general radiological findings
- evidence of active or inactive TB disease
The CXR must contain the following information:
- applicant’s name
- applicant’s date of birth
- applicant’s gender
- date of the chest x-ray
Applicants must bring their IME number, UMI number and UCI number with them to undergo their CXR. Panel radiology clinic staff will use these numbers or the applicant’s name and passport number to retrieve the applicant’s health case in eMedical.
If an applicant is pregnant for the CXR
There may be cases where an applicant is not pregnant for the IME, but is pregnant for the x-ray examination. If an applicant is pregnant and elects to proceed with the CXR examination with adequate pelvic lead shielding, there are no changes to the CXR procedures.
If the client chooses to defer her CXR because of pregnancy:
- IRCC is informed electronically by eMedical that the client is pregnant, along with her estimated date of delivery
- eMedical generates a pregnancy deferral letter with instructions for the client
- the IME is put on hold status until the chest x-ray has been completed
- the IME is submitted to IRCC along with the CXR results when they become available
CXR indicating active tuberculosis
When a panel radiologist indicates suspected active TB in the applicant’s CXR, they notify the panel physician. As the panel physician, you must do the following:
- Arrange immediately for the client to undergo sputum testing.
- For confirmed, active TB cases, notify the public health authorities according to the country’s or region’s public health guidelines and directives.
- Submit the health case in eMedical within the service standard, including all reports available. The RMO will instruct you if further examinations are required.
For all confirmed, active pulmonary TB cases, you must also:
- conduct screening for HIV, if not already done
- proceed with contact screening as per the tuberculosis technical instructions for all family members or close contacts who are also IRCC clients
- recommend that non-IRCC close contacts see their own physicians for screening
- recommend that all contacts receive treatment for latent TB, as per IRCC's technical instructions.
Panel Physicians should notify the RMO as soon as possible if IMEs have already been completed and submitted for family members who require contact tracing.
As a result of contact tracing, applicants discovered to have latent TB should be reviewed by a local TB specialist to determine if treatment is recommended.
See IRCC's technical instructions for more information.
Radiology grading
Before submitting the CXR, the radiologist must provide a grading for the image.
- The system will automatically provide a radiology grade based on the reported findings.
- Grade A indicates that there is no evidence of TB or abnormalities suggestive of other significant diseases identified.
- Grade B indicates that there is evidence of TB or abnormalities suggestive of other significant diseases identified.
- If the system has provided an A grade and the radiologist believes that there is evidence of TB or abnormalities suggestive of other significant diseases, they may change the grade to B.
- If the system has provided a B grade, it cannot be changed to an A grade.
- No comments are permitted for A-grade CXRs.
- Comments are mandatory for B-grade CXRs.
Panel Radiologist Declaration
The radiologist declaration confirms the following:
- The client’s identity has been verified.
- The radiology report is an accurate record of the radiologist’s findings.
Important information:
- Panel radiologist declarations are provided electronically.
- Radiology support staff can declare on behalf of a panel radiologist.
Submitting CXRs
- Digital CXRs are uploaded to the eMedical system.
- The radiologist or authorized radiology support staff enter the general and special findings in the eMedical system.
- The CXR is graded in the eMedical system and submitted to the client’s IME.
- The panel physician’s clinic is notified that the CXR examination has been completed.
- The panel physician reviews the radiologist report and grading.
- Once all examinations are completed, the panel physician submits the IME to IRCC.
Resettlement Needs Assessment (Exam 948 in eMedical)
When an applicant is being processed as a refugee overseas, the migration office issues a Medical Report: Client Biodata and Summary (IMM 1017) with the IMM category of “refugee overseas”.
In such cases, the Resettlement Needs Assessment is included in the medical instructions sent to the applicant by a migration office as part of the IME.
The form is available electronically under section 948 in eMedical. Panel physicians must complete this section for all applicants in the refugee overseas category. Please note that, for privacy reasons, this form must only indicate the anticipated services for the applicant and not provide medical information or a diagnosis.
See IRCC's technical instructions under Resettlement Needs Assessment for detailed instructions on how to complete the form.
Pregnant Client – X-Ray Deferred
If the client chooses to defer her chest x-ray (CXR) because of pregnancy, the following steps apply:
- eMedical informs IRCC electronically when a CXR is deferred. The health case is put on hold when an applicant is pregnant and chooses to defer her CXR.
- eMedical generates a CXR requisition and instructions, which are then provided to the applicant.
- eMedical generates a “Pregnancy Deferral Letter” with instructions for the applicant.
- The panel physician completes all other components of the IME, checks the box for “pregnancy” and submits the IME in eMedical. Migration officers can see the status of the IME in GCMS: “On HOLD pregnancy” until the CXR is completed.
- The IME will be submitted to IRCC along with the CXR results when they are available for assessment by the RMO.
If the applicant is undergoing an upfront medical examination, then the applicant must be given a copy of the form Upfront Medical Report – Client Biodata and Summary (IMM 1017B upfront) so they can submit it with their visa application before undergoing the post-partum CXR.
Additional forms for the IME
See Appendix III for samples of the following additional forms:
- IMM 5725 or Exam 903 in eMedical: Activities of Daily Living (ADL)
- IMM 5738 or Exam 904 in eMedical: Chart of Early Childhood Development (CECD)
- IMM 5728: Acknowledgment of HIV Post-Testing Counselling
You must print out, sign and scan this form when promoted by eMedical.
- IMM 5734: Specialist’s Referral Form
The panel physician will send most referrals electronically. You may print the letter if the applicant requests a printer version, or for any other reason you wish.
Additional information for submitting IME forms
IME grading: Grade A or Grade B
Before you submit the IME, you must provide a grade for it. The system will automatically provide an IME grade based on your reported findings:
- Grade A indicates that there are no abnormal findings present and no significant abnormal history.
- Grade B indicates that there are significant abnormal findings present and/or an abnormal history.
- If the system has provided an A grade and you believe there are significant abnormal findings, you may change the grade to B.
- If the system has provided a B grade, you cannot change it to an A grade.
- No comments are permitted for A grade IMEs.
- Comments are mandatory for B grade IMEs.
Panel physician declaration
The panel physician’s declaration is provided electronically. It confirms the following:
- You have verified the applicant’s identity.
- The IME and medical report are an accurate record of your findings.
Furtherance process
RMOs may need more information to complete their medical assessment. They get this through the furtherance process. Furtherance might create additional costs for the applicant, including additional tests and specialist evaluation.
As the panel physician who did the original IME, you are responsible for the following:
- Refer the applicant for additional testing to another panel physician, or to an appropriate specialist for consultation. (You, not the applicant, are responsible for selecting the specialist.) The applicant’s previous medical records may be provided along with the additional reports requested by the RMO.
- Complete the furtherance requirements by reviewing the new medical results and ensuring they respond fully to the original furtherance request, then submitting the results to the RMO. If the new medical result does not respond fully to the original furtherance request, provide a written explanation as to why.
Here are the next steps of the process:
- The RMO issues a letter to the applicant with instructions to return to a panel physician for further investigations.
- The furtherance request is transferred to eMedical.
- You retrieve the furtherance request from eMedical by carrying out a search using the IME or UCI number indicated in the client’s letter.
- You complete the additional examination(s) or generate a referral letter with the information that will be sent to a specialist for the required investigation(s).
- You enter the information into eMedical and submit the information to IRCC.
Panel members who work in Canada
This section of the guide provides information, instructions and reference material for panel members operating in Canada. It does not apply to panel members who perform Canadian IMEs in other countries.
Providing primary care for IME applicants
If you are asked to provide treatment to an applicant or provide a medical opinion outside the IME, you should make sure the applicant understands the different duties and responsibilities of a third-party physician (i.e. a panel physician) versus a treating physician. For example, if you recommend a treatment that is not mandatory for immigration purposes, the applicant must understand this.
The provincial and territorial medical licensing authorities give doctors guidance on the difference between a treating and third-party physician. Applicants should also understand that any medical services not related to the IME or covered under the Interim Federal Health Program do not involve IRCC.
Providing services in Canada’s official languages
IRCC is committed to providing applicants in Canada with service in their preferred official language: English or French. If your clinic cannot provide service in the applicant’s official language of choice, you should refer them to the nearest panel physician who can. If no such physician exists nearby, you should ask the applicant to contact IRCC’s Call Centre at 1-888-242-2100, or consult IRCC’s website.
Protection of personal information
Several Canadian statutes protect people’s personal information. They include:
- the Privacy Act
- the Access to Information Act
- the Canadian Charter of Rights and Freedoms
- the Library and Archives Act
- the Personal Information Protection and Electronic Documents Act (PIPEDA)
- Various provincial and territorial privacy laws
As a panel physician, you must follow these laws when you collect, use, disclose, retain and dispose of people’s personal information. It is critical, for example, to collect and store personal information in a way that protects it from unauthorized disclosure.
The laws of other jurisdictions where information is collected may also apply to your treatment of applicants’ personal information.
To comply with legislation, the IME forms sometimes require applicants to consent to the disclosure of their personal health information to third parties.
Panel physicians in Canada can get advice from their professional organizations or regulating bodies on how to apply the Personal Information Protection and Electronic Documents Act (PIPEDA) and provincial or territorial privacy legislation, as well as how to properly manage personal information.
Refugee determination system in Canada
Refugee claimants – more appropriately called “asylum seekers” – are individuals who, after they arrive in Canada, make a formal claim to an IRCC or Canada Border Services Agency officer asking for Canada’s protection.
Under the Immigration and Refugee Protection Act (IRPA), all people seeking asylum must get an IME. They are referred for an IME when they make their claim. The IME forms and requirements for asylum seekers are the same as for other immigrants. They are given medical instructions and a list of panel physicians. They must undergo their IME within 30 days following their claim for asylum.
Immigrants are examined to identify medical conditions that might affect their admissibility to Canada under IRPA. Asylum seekers fall under the excessive demand exempt (EDE) category. This means they are examined primarily to identify conditions that might pose risks to public health and public safety; however, any additional services required by IRCC's technical instructions may also be provided.
Asylum seekers who have been granted protected person status by the Canadian authorities are entitled to health care under the Interim Federal Health Program (IFHP) until they become eligible for provincial or territorial health care coverage. This means their first IME is covered. If they must undergo a second IME, it is not covered under the IFHP.
Your duty to report tuberculosis
Individuals whose IME shows they have inactive tuberculosis are placed under medical surveillance in Canada. The Public Health Liaison Unit (formerly known as the Medical Surveillance Unit) reports such cases to the appropriate provincial or territorial public health authorities.
However, as a panel physician, you are also required to notify the appropriate provincial or territorial public health authorities of such cases according to the laws of the province where you practice.
At no time should routine investigation or management of active or suspected active tuberculosis be deferred or delayed because of immigration medical activities. If you cannot contact an applicant suspected of having an active notifiable infectious disease such as tuberculosis, you should immediately inform the IRCC Migration Health Branch.
The Interim Federal Health Program (IFHP)
IFHP for panel members working in Canada
The IFHP provides limited, temporary coverage of health care benefits in Canada to groups not eligible for provincial or territorial health insurance, such as resettled refugees, refugee claimants, victims of human trafficking and individuals detained under the Immigration and Refugee Protection Act.
IFHP covers the costs of services and products to eligible beneficiaries in Canada as indicated in the IFHP benefit grids. It is important to note that, in Canada, the IFHP only covers the cost of one IME and related tests.
The IFHP’s claims administrator, Medavie Blue Cross, adjudicates and pays claims for the program.
Panel members must register with IFHP
A panel member or any service provider assisting with IME-related tests must register as an IFHP Provider and comply with the terms and conditions of Medavie Blue Cross.
Please refer to the IFHP Benefit Grid – IME and IME tests available on the Medavie Blue Cross website for more information on the services, diagnostic tests, and the maximum dollar amount.
Verifying IFHP eligibility
-
Eligibility documents
There are three types of documents that show that an individual may be eligible under IFHP in Canada. Individuals must show one of these documents to their health care provider at each visit:
- Refugee Protection Claimant Document (RPCD)
- Interim Federal Health Certificate (IFHC)
- Acknowledgement of Claim and Notice to Return for Interview letter (AOC)
-
Confirm eligibility with Medavie Blue Cross
Panel physicians must confirm with Medavie Blue Cross that the individual’s coverage is active before the examination is carried out. It is important to note that it takes two business days for the IFHP eligibility to be reflected in the Medavie Blue Cross system. However, beneficiaries are still eligible during this two-day period. When an IFHP client asks for your services within two business days of the date on the IFHP eligibility documents, you must:
- review the “effective date” on the eligibility document to confirm that it is within the two business-day period
- provide the services and delay submitting the invoice to Medavie Blue Cross until the coverage has been updated in their system
Additional information
Please see the IFHP Information Handbook for Health Care Professionals (PDF, 7 MB) for more information. The handbook is available on the Medavie Blue Cross website, where you can find the IFHP Benefit Grids and more information about the IFHP, including:
- prior approval procedures
- claim submission guidelines
- provider terms and conditions
- payment procedures
- important information on how to perform IMEs for refugee claimants in Canada
IFHP for panel members working overseas (pre-departure medical services)
On April 1, 2017, the IFHP was expanded to cover certain pre-departure medical services (PDMS) for Canada-bound resettled refugees before they come to Canada.
The claims administrator for the IFHP, Medavie Blue Cross, administers claims submitted by health care providers and secondary care providers such as hospitals, laboratories and specialists who have provided services to individuals eligible for PDMS. More information on PDMS is available on the Medavie Blue Cross website.
Groups and individuals eligible for PDMS
The following are eligible for PDMS:
- individuals identified for resettlement to Canada (i.e. government-assisted asylum seekers)
- privately sponsored asylum seekers
- blended migration office-referred asylum seekers
- groups or individuals who have been specially designated by the Minister of IRCC
- certain people who are being resettled in Canada as a result of a public policy or on humanitarian and compassionate grounds as determined by the Minister of IRCC
Registering for PDMS
Panel members – whether or not they are affiliated with the International Organization for Migration (IOM) – should register with the IFHP through Medavie Blue Cross.
IOM-affiliated panel members must register with the IFHP; however, they will receive reimbursements for their services directly from IOM. They are not required to submit the claims for reimbursements to Medavie Blue Cross.
Non-IOM affiliated panel members are required to register with the IFHP and claim reimbursement for their services directly from Medavie Blue Cross.
To learn more about the registration process, see the IHFP Handbook for Pre-Departure Medical Services (PDMS) Providers (PDF, 5.1 MB).
PDMS coverage and benefits
The scope of the IFHP PDMS coverage is limited to:
- the cost of the Immigration Medical Examination (IME) and follow-up treatment for health conditions that would affect an individual’s medical admissibility to Canada (i.e. active tuberculosis and untreated syphilis)
- communicable disease prevention and control by providing vaccinations that are aligned with Canadian immunization guidelines
- medical support required during travel to Canada includes medical attendant and/or medical devices (e.g. oxygen, wheelchairs)
- management and control of communicable diseases in refugee camps
Please see the IFHP Benefit Grid for PDMS (PDF, 357 KB) for a list of eligible services and additional information.
Pre-departure vaccination services
Panel physicians affiliated with the International Organization for Migration (IOM), can provide certain vaccination services covered by the IFHP to eligible individuals. This service is voluntary and does not impact their application for resettlement to Canada.
Immunizations can be provided only in countries where the IOM has the capacity to deliver vaccinations. The Immunization Manual (1.5 MB) contains more information including:
- standard operating procedures
- vaccine administration and schedule
- consent form and vaccination documentation worksheet
Medical support in transit
The costs related to medical support in transit (medical attendant and/or medical devices) are covered by the IFHP. A prior approval request (PDF, 178 KB) must be sent to the IFHP Unit (IRCC.IFHP-PFSI.IRCC@cic.gc.ca) with the provider’s Regional Medical Office (RMO) in cc. The request must include clinical information and recommendations for medical support in transit with detailed medical services, devices or products required and expected cost.
If approved, an IFHP officer will sign and return Part 1 (administrative) of the form to the requestor. For more information or questions, please contact IRCC.IFHP-PFSI.IRCC@cic.gc.ca.
You can find the Medical Support in Transit Form (PDF, 226 KB) (prior approval request) on the web site of the IFHP Claims Administrator Medavie Blue Cross.
Outbreak response
When a communicable disease outbreak occurs in a refugee camp, the IFHP will reimburse services and products related to the following:
- diagnostic testing (rapid and serologic)
- post-exposure prophylaxis (vaccines and drug therapy)
- pre-departure health screening and personnel cost, including the cost of physician and nursing visits.
The costs related to the management and control of an outbreak are covered by the IFHP. A prior approval request must be sent to the RMO as soon as an outbreak is identified by the PP/IOM. Please note that the request will also be reviewed by the IFHP Unit to ensure compliance with the IFHP Policy. The request must include the following information:
Location and description
Provide a short description of population demographics and a description of the area/facility where the outbreak has occurred (i.e. camp, region, province, country, etc.)
Confirmation of an outbreak
Your description should include the following:
- epidemiological case definition
- case finding
- lab confirmation (if any)
- how the outbreak was initially reported and steps taken to confirm it
- how serious the outbreak is (potential for spread, mortality and complications)
- number of cases and particular groups at risk among those identified for resettlement to Canada
- how soon the individuals will be traveling to Canada
Ongoing action (capacity)
Provide a brief description of the current response and capacity, including the investigations done and control measures taken (human, medical, etc.)
Proposed response
What should be done to control this outbreak? Propose the control activities and supplies needed (medicines, materials) and the expected cost per individual, including:
- treatment of cases and carriers
- isolation of cases
- surveillance of suspects
- immunizations:
- Obtain all immunization records (consult IFHP Vaccination Documentation Worksheet (PDF, 321 KB), if available).
- Identify required vaccine(s) and number of doses.
- Confirm the vaccine cost per dose, including the administration cost.
- chemoprophylaxis
- personal protection
- environmental hygiene
- personal hygiene
- disinfection and sterilization
- pre-departure screening
- other
For claims-related instructions please consult the provider handbook.
Verifying IFHP eligibility for PDMS services
It is your responsibility as a panel physician to confirm an individual’s eligibility to the IFHP before services are rendered. This is an important aspect of protecting the integrity of the program.
Non-IOM affiliated providers must complete the following procedures:
- confirm that the individual has an IFHC
- confirm that the identity of the individual on the IFHC matches the individual in the identification document
- retain a photocopy of the individual’s IFHC in their records
IOM-affiliated providers will do the following procedures to confirm an individual’s eligibility:
- confirm that the individual’s name appears on the list received from IRCC visa offices
- confirm that the identity of the individual matches the individual in the identification document
- retain a copy of the list of eligible individuals received from IRCC visa offices
Important: If you have questions related to an individual’s eligibility, please contact Medavie Blue Cross at CIC_Inquiry@medavie.bluecross.ca, including the individual’s UCI and the benefit code.
For more information, please see the PDMS provider handbook (PDF, 5.1 MB).
Claim submission guidelines for in-Canada or overseas services
You have up to six months after providing your services to submit invoices to either the IOM or Medavie Blue Cross. When you submit claims for IMEs and related tests, you must use current IFHP benefit codes, which you can find in IFHP Benefit Grid – IME and IME tests available on the Medavie Blue Cross website (for panel members working in Canada) or the Benefit Grid for PDMS (PDF, 357 KB) (for panel members working overseas).
Here are some key elements of IFHP’s fee policy:
- Your compensation is based on a fee-for-service model. The IFHP fee policy is to reimburse physicians according to usual and customary fee rates in place on the date of service or according to fee rates established by the IFHP.
- You must not collect from the client the difference between the total amount billed for the services and the amount to be reimbursed by Medavie Blue Cross, if any.
- The IFHP is not designated to reimburse beneficiaries directly. Do not directly charge patients covered by the IFHP. If a beneficiary pays you directly for services or products covered by the IFHP, they cannot be reimbursed.
- You may not refuse to provide IMEs for individuals covered by the IFHP. However, you may charge for missed appointments according to your local standards of practice. This charge will not be reimbursed under the IFHP.
- You must accept whatever method of payment an applicant wishes to use. In addition, the services you provide must not be influenced by whether the service is a covered benefit for the client.
Section 2: Supplementary Information
Instructions for completing paper-based IMEs
This section provides panel members who use a paper-based system with information they need to complete IME and associated forms.
Panel members using eMedical should refer to The Immigration Medical Examination section of this guide.
IME paper forms have been redesigned to ensure they are consistent with eMedical IMEs.
General information about the IME
The IME consists of a medical history, physical examination, age-specific laboratory tests and age-specific chest x-ray.
Usually, routine, age-specific laboratory and radiologic tests include:
- urinalysis – applicants age 5 and older
- chest x-ray (posterior-anterior view) – applicants age 11 and older
- syphilis – applicants age 15 and older
- HIV – applicants age 15 and older
- serum creatinine – applicants age 15 and older
A medical examination includes any or all of the following:
- physical examination
- mental examination
- review of past medical history
- laboratory test
- diagnostic test
- medical assessment of records respecting the applicant
- urinalysis – applicants age 5 and older
- chest x-ray (posterior-anterior view) – applicants age 11 and older
- syphilis – applicants age 15 and older
- HIV – applicants age 15 and older
- serum creatinine – applicants age 15 and older
Panel members may request additional lab tests based on an applicant’s individual risk factors.
It also be necessary to screen applicants below the ages indicated. See IRCC's technical instructions for more information.
How do I determine what examinations are required?
As the panel physician, you are never required to decide on a course of treatment or additional tests for an applicant. Your regional medical office (RMO) will contact you with the specifics of the applicant’s case and the medical examinations they require. You must follow the technical instructions for all tests and procedures.
Getting your unique identifier and login
Once IRCC has received all your forms and documents, your RMO will tell you that you are approved as a panel member. You will get a unique identifier number (P number), which enables IRCC to perform quality assessments of your work.
The unique identifier starts with the letter “P” followed by eight or more digits (e.g. P12345678).
For panel members or their locum tenens performing a paper-based IME, the unique identifier, along with their name, must be clearly readable on the front page of each Medical Report – Client Biodata and Summary (IMM 1017) as well as on the “Laboratory Requisition and Report” and “Chest X-Ray Requisition Report” sections of the IMM 5419: Medical Report form.
The panel member or their locum tenens must clearly indicates their name, the P number, the city and the country in all correspondence with IRCC. For example:
- Name:
- P#:
- City, Country:
Each photo attached to the Medical Report – Client Biodata and Summary (IMM 1017) must be signed to confirm the identity of the applicant. Make sure that each IME is signed properly. In cases where the IMEs are not properly signed, the RMO can refuse them and return the IMEs to the panel physician’s office.
Panel radiologists may embed this information on the chest x-ray along with other required information about the client.
For IMEs sent by mail or courier, the value on any customs declaration should state “No commercial value”.
Reporting contact information and absences
- Panel members and clinics that have been approved by their RMO to use paper-based forms must actively inform the RMO of any changes in their contact information.
- When you are absent from IME activities, the RMO will update the information in your record to track the leave.
- When you use a locum tenens, the locum must sign the Medical Report – Client Biodata and Summary (IMM 1017) “for and on behalf for Dr. , ”. The locum must also use their personal wet stamp.
- You must forward an inactive immigration medical file to your RMO within eight weeks of initiating an IME.
Guidelines for managing paper records
Original documents and information related to an IME must be forwarded by the panel physician or a trusted employee to their RMO by regular mail or commercial courier and must never be given to the applicant or their representative for delivery to the RMO.
You are encouraged to give a copy of the IME to the applicant (or their guardian) unless there is a strong reason to not do so (e.g. information from a different applicant is found within the IME or releasing the information would reasonably lead to another person or entity being subject to significant inappropriate behaviour by the client.
You must keep copies and records of files for two years or longer if required by your local medical regulatory authority. Remember, you can access the IME in eMedical for only 365 days after submitting the case.
Fees for IMEs
If you are completing a paper-based IME that must be mailed to the RMO, you should discuss the method and cost of sending the documents with the applicant beforehand.
Verifying an applicant’s identity
It is essential that you identify applicants throughout the IME process to ensure the person undergoing the IME is the same person applying for entry to Canada, and that there is no substitution at any time during the lifecycle of the IME. An applicant’s identity is confirmed through a process of verifying the applicant’s photographs and identity documents.
Obtain photos of the applicant
- The applicant must provide four recent photographs to the panel clinic.
- Photographs must meet IRCC’s photographic specifications standards (PDF, 506 KB).
- If the photographs do not meet the specifications, ask the applicant to provide new photographs before you complete the IME.
What to do with the photos:
- You must attach photos to the Medical Report – Client Biodata and Summary (IMM 1017) as well as on the “Laboratory Requisition and Report” and “Chest X-Ray Requisition Report” sections of the IMM 5419: Medical Report form.
- When your clinic uses these photos, it must confirm that the photos are a true and recent likeness of the applicant being examined.
- You must signed the photograph on the Medical Report – Client Biodata and Summary (IMM 1017) in the top right corner with your panel physician’s ID.
If you have an identity concern
If you cannot confirm that the person who has arrived for an IME is the person on the ID documents being presented – or if the applicant provides personal details that seem inconsistent with the information on the identity documents they submit – you should report that as an ID concern.
Attach photocopies of the identification document in question to the IME and submit it to IRCC.
IRCC will investigate your concern about the applicant’s identity.
Required documents
The applicant must submit a passport or other identification document acceptable for the Canadian IME. IRCC strongly prefers that applicants submit passports. This includes new passports and passports expired for no more than a year.
Other approved identification documents include the following:
- national ID card (an original birth certificate is an acceptable national ID document for minors under the age of consent only)
- driver’s licence (Canadian licences only)
- refugee travel document
- Red Cross travel document
- UN laissez-passer
- Seaman’s book
- Organization of American States travel document
- Refugee Protection Claimant Document
If an applicant does not have approved identification
If an applicant does not provide an approved identification document, they must provide an alternative form of identification. You should not turn such applicants away, and should conduct the IME as long as the applicant presents some form of identification.
If the applicant provides identification that is not approved, or if you have doubts about the authenticity of the document presented, you must report your concern on the Medical Report – Client Biodata and Summary form (IMM 1017). A copy of the identity document of concern should be attached to the IME.
Important: To ensure the integrity of the IME process, the applicant must use the same identity document for all components of the IME, including laboratory, radiology and specialist referrals. Please inform your clients accordingly.
Client Declaration and Notice
(See our sample Client Declaration and Notice form in Appendix II.)
Before undergoing an IME, all applicants must complete the Client Declaration and Notice form. A legal guardian or parent may provide and sign the declaration on behalf of the applicant if the applicant is under 16 years of age or is unable to complete and sign the declaration for reasons of incompetency (for example, if they have reduced mental capacity).
The Client Declaration and Notice form for paper-based IMEs includes the following:
- a declaration stating that all information provided at the time of the IME is true and complete
- a notice stating that the IME information will be collected and temporarily stored in the eMedical system on segregated databases located in Australia
- a notice explaining that the collection, use and disclosure to IRCC of IME information follows Canada’s Immigration and Refugee Protection Act or protects the health and safety of Canadians
- a notice explaining the collection, storage, use and disclosure of vaccination information where the applicant has consented to the disclosure of this information to IRCC
Other important details:
- The applicant must sign the copy of the Client Declaration and Notice provided by you or your staff. Forms that have been altered or translated into another language are not acceptable.
- You or your staff should review the Client Declaration and Notice form with the applicant and answer any questions.
- Clinic staff must attach the form and submit it along with the IME.
- The IME must not be submitted to your RMO without a completed Client Declaration and Notice form.
- The Client Declaration and Notice form is not a consent document and should not be construed as consent for the purpose of the IME or for vaccination.
- You must ensure to obtain client consent according to your country’s guidelines or legal requirements before performing medical tests and procedures required for the IME and before administering any vaccination, where applicable.
- You must ensure that the applicant understands and accepts that any relevant personal information collected during the IME process, including IME information and any vaccine-related information, when applicable, will be disclosed to IRCC.
- If an applicant does not complete the Client Declaration and Notice form, you cannot carry out the IME and you must notify your RMO.
- The applicant (or legal guardian/parent) must sign and date the Client Declaration and Notice form.
Medical Report: Client Biodata and Summary (IMM 1017)
(See our sample IMM 1017 form in Appendix III.)
IRCC has implemented one standard form, the Medical Report – Client Biodata and Summary (IMM 1017), for all immigration categories. This form displays information such as:
- client information (biodata)
- immigration information
- IMM type: excessive demand exempt (EDE), non-EDE, refugee
- IME grading
- panel physician declaration
Excessive demand exempt (EDE) applicants
EDE applicants are people who cannot be deemed inadmissible on the grounds that they would place an excessive demand on publicly funded Canadian health and social services. EDE applicants include refugees, refugee claimants, individuals with protected person status, and certain clients in the family classes.
However, EDE clients are assessed for:
- danger to public health
- danger to public safety
Non-EDE applicants
Non-EDE applicants are assessed for:
- danger to public health
- danger to public safety
- excessive demand on publicly funded Canadian health and social services
Refugee overseas applicants
Refugee overseas applicants are automatically assessed as EDE. Panel physicians must complete and submit the Resettlement Needs Assessment Form (IMM 5544) for overseas refugees.
IRCC typically issues the Medical Report – Client Biodata and Summary (IMM 1017) form with the applicant’s information and immigration information sections completed.
Applicants who have been issued a Medical Report – Client Biodata and Summary (IMM 1017) must present the form to your clinic when they arrive for their IMEs. The form will include two applicant identifiers: IME number and UCI number. (Note: This form may not include a client photo).
Here are the steps you should take as a paper-based clinic:
- Confirm the applicant’s identity by comparing the applicant’s information with the approved identification document.
- Attach a recent applicant photo (provided by the applicant) to the Medical Report (IMM 1017).
- Complete and submit the Medical Report (IMM 1017) along with all other IME forms.
Upfront Medical – Client Biodata and Summary (IMM 1017B upfront)
(See our sample IMM 1017B upfront form in Appendix III.)
An upfront medical is an IME performed when an applicant reports to a panel physician with no paper Client Biodata and Summary (IMM 1017) or file in the eMedical system. Upfront medical examinations are generally permitted for students and workers who are applying to be temporary residents of Canada.
Only certain applicants are permitted to undergo an upfront medical.
These exams do not apply to family members being sponsored by a permanent resident of Canada. Whenever IRCC makes changes to the rules about individuals who can undergo an upfront medical, panel physicians are notified by their RMO.
When you complete this form, you must use the IMM 1017B upfront paper forms that have been provided to you. They are pre-populated with a UMI number and a barcode.
Here are the steps your clinic and staff must take:
- Check the applicant’s identity with a valid, government-issued ID.
- Attach a photo of the applicant (provided by the applicant) to the form.
- Select the immigration category by checking the appropriate box (usually student or worker).
- Complete page 1 of the IMM 1017B upfront form “Copy to Client” and give it to the applicant so they can submit it to IRCC along with their visa application.
- Complete page 2 of the IMM 1017B upfront form “Copy to Health Branch” and submit it to your RMO along with all other IME forms (e.g. IMM 5419, chest x-rays, lab results, etc.).
Note: It is very important to ensure the correct page goes to the client and the correct page goes to your RMO:
- Page 1 — Client
- Page 2 — RMO
Panel physicians must ensure they provide the applicant with proof that they have competed their upfront medical examination. For paper-based upfront medicals, it is the top page of the Upfront Medical Report – Client Biodata and Summary (IMM 1017B upfront) form. Applicants must include this proof when they submit their visa application.
Since an IME is valid for 12 months, you should remind applicants to submit their visa application along with proof that they have completed their upfront medical examination well before the expiration date; otherwise, the client may have to undergo a second IME.
Medical Report (IMM 5419)
You will use the applicant’s medical report to assess their medical condition. The medical report may be completed by clinic staff or the applicant, but you as the panel physician must review it to confirm the information.
You must provide details along with all “Yes” answers to medical history questions. IRCC requires the following information:
- date of diagnosis
- date of treatment or surgery
- relevant medications
- current status of the condition (and, if applicable, the prognosis)
You must either provide this information in the comments section or attach a report to the IME.
The following table lists additional requirements when the answers to medical report questions show abnormality – whether the IME is completed in eMedical or on paper. Refer to IRCC's technical instructions for more information.
Medical history questions
| Question | Related TI | IMM type | Requirements if abnormal |
|---|---|---|---|
| Tuberculosis (TB), treatment for tuberculosis | Tuberculosis TI | EDE and non-EDE clients | Lateral CXR & AP CXR if < 11 years old, Chest x-ray examination |
| Close household or work contact with tuberculosis (within last 5 years) | Tuberculosis TI | EDE and non-EDE clients | IGRA or TST, lateral CXR & AP CXR if < 11 years old, Chest x-ray examination |
| Prolonged medical treatment and/or repeated hospitalization for any reason, including a major operation or mental illness | N/A | EDE and non-EDE clients | Medical report, if available when IME is submitted or if RMO requests |
| Psychological/psychiatric disorder (including major depression, bipolar disorder or schizophrenia) | Psychiatric conditions TI | EDE and non-EDE clients | Report from psychiatrist, psychologist or treating physician (attach all existing results and reports from labs and previous specialists) |
| History of HIV | HIV TI | EDE and non-EDE clients | HIV, CXR, Hepatitis B and C, syphilis, IGRA or TST regardless of age, and HIV specialist report including CD4 count, HIV viral load, and when antiretroviral medications will be needed |
| An abnormal hepatitis B or C blood test | Hepatitis / Liver disease TI | EDE and non-EDE clients | HIV, CXR, Hepatitis B and C, syphilis, regardless of age |
| Cancer or malignancy in the last five years | Cancer or Malignancy TI | non-EDE clients | Oncology report |
| Diabetes | Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Screen for signs or symptoms and presence of end-organ damage. |
| Heart condition including coronary disease, hypertension, valve or congenital disease | Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Screen for signs or symptoms (including blood pressure) and presence of end-organ damage. Serum creatinine, regardless of age |
| Blood condition (including thalassemia) | N/A | non-EDE clients | Check for history of admission. |
| Kidney or bladder disease | Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Urinalysis, serum creatinine (eGFR if abnormal); regardless of age |
| An ongoing physical or intellectual disability affecting current or future ability to function independently or be able to work full-time (including autism or developmental delay) | Psychiatric conditions TI and Cognitive impairment in adults TI | EDE and non-EDE clients | ADL if > 5 years old, CECD if < 5 years old, consult TI for complete requirements |
| Addiction to drugs or alcohol | Psychiatric conditions TI | EDE and non-EDE clients | Only if the RMO requests – a psychiatrist’s, psychologist’s or treating physician’s report that specifically comments on previous threatening behaviour and if there is evidence of IV drug use, HIV, hepatitis B and C, regardless of age. The report must also specifically address if it is reasonably likely the client will exhibit future behaviour that might be a threat to the client or others. |
| Prescribed pills or medication (excluding oral contraceptives, over- the-counter medication and/or natural supplements) | N/A | EDE and non-EDE clients | List relevant medications and mention the indication |
| For female clients: a) Are you pregnant? |
N/A | EDE and non-EDE clients | N/A |
| b) If yes, what is the expected date of delivery? | N/A | N/A | N/A |
| c) If yes, do you wish to defer your chest x-ray at this time? | N/A | N/A | Attach IMM 5733 Instructions for Pregnant Client – X-Ray Deferred |
Physical Examination
As the panel physician, you must complete the physical examination. You must provide details of all abnormal findings during the physical examination. IRCC requires the following information:
- history
- diagnosis
- treatment details (including dates and medications)
- lab results
- specialist reports (as required)
- current status
- prognosis
You may enter this information in the comments section or attach a report to the IME.
The following table lists additional requirements when the answers to physical examination questions show abnormality. See IRCC's technical instructions for more information.
Table: Physical Examination
| Physical examination | Related TI | IMM type | Requirements if abnormal |
|---|---|---|---|
| Was a chaperone offered? | Genital, Gynecological and rectal examination TI; Breast examination TI | EDE and non-EDE clients | Non applicable. A chaperone should be offered to everyone. |
| Ear/nose/throat/mouth | N/A | EDE and non-EDE clients | N/A |
| Hearing | Hearing impairment or deafness TI | EDE and non-EDE clients | N/A |
| Eyes (including fundoscopy) | N/A | EDE and non-EDE clients | N/A |
| Best distance visual acuity (with or without correction) | N/A | EDE and non-EDE clients | N/A |
| Blood pressure (clients = 15 years of age) Normal readings
|
Diabetes, hypertension, chronic renal or cardiac diseases TI | EDE and non-EDE clients | Repeat blood pressure |
| Repeated blood pressure (clients = 15 years of age) Normal readings
|
Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Screen for signs or symptoms (including blood pressure) and presence of end-organ damage serum creatinine regardless of age |
| Cardiovascular system | Diabetes, hypertension, chronic renal or cardiac diseases TI | non-EDE clients | Serum creatinine, regardless of age, |
| Respiratory system | Tuberculosis TI | EDE and non-EDE clients | If signs of TB: CXR, HIV, screen for hepatitis B and C, regardless of age |
| Nervous system: sequelae of stroke or cerebral palsy, other neurological disabilities | Debilitating conditions, Activities of daily living, and/or Developmental milestones: Chart of early childhood development TIs | EDE and non-EDE clients | Complete Activities of daily living, Development milestone: Chart of early childhood development and/or an assessment of cognitive functioning forms |
| Mental and cognitive state | Cognitive impairment, Activities of daily living, and/or Developmental milestones: Chart of early childhood development TIs | EDE and non-EDE clients | ADL if > 5 years old, CECD if < 5 years old, consult TI for complete requirements |
| Intellectual ability | Cognitive impairment, Activities of daily living, and/or Developmental milestones: Chart of early childhood development TIs | EDE and non-EDE clients | ADL if > 5 years old, CECD if < 5 years old, consult TI for complete requirements |
| Developmental milestones (clients = 5 years of age) | Developmental milestones: Chart of early childhood development TI | EDE and non-EDE clients | Complete Developmental milestones: Chart of early childhood development form |
| Gastrointestinal system | Hepatitis/liver disease TI | EDE and non-EDE clients | |
| Musculoskeletal system | Debilitating conditions TI and Activities of daily living TI | EDE and non-EDE clients | Complete activities of daily living if > 5 years old, CECD if < 5 years old |
| Skin and lymph nodes | Cancer and HIV TI | EDE and non-EDE clients/td> | Screen for skin cancer, leprosy, surgical scars, tattoos and piercings. Inspect/palpate neck, axilla and groin for lymphadenopathy |
| Evidence of substance abuse (e.g. venous puncture marks) | Psychiatric conditions TI | EDE and non-EDE clients | Complete psychiatrist’s report and, if evidence of IV drug use HIV, hepatitis B and C screening, regardless of age |
| Endocrine system (such as evidence of complications from diabetes) | Diabetes, hypertension, chronic renal and cardiac diseases TI | non-EDE clients | If diabetes is present, proceed with screening. |
| Are there any physical or mental conditions that may prevent this person from attending a mainstream school, obtaining full-time employment or living independently now or in the future? | Psychiatric conditions and Cognitive impairment TI | EDE and non-EDE clients | ADL if > 5 years old, CECD if < 5 years old, consult TI for complete requirements |
| Breast examination | Genital, gynecological and rectal examination TI | EDE and non-EDE clients | Investigate (e.g. ultrasound, mammogram, specialist report) |
Laboratory Requisition and Report
Here are the general instructions for completing this report:
- Complete the Laboratory Requisition and Report (IMM 5419), entering the applicant’s personal information:
- surname
- given name
- date of birth
- IME number or UMI number, if applicable
- Attach the applicant’s photograph to ensure the integrity of the IME for laboratory testing.
- Indicate with a checkmark (R) the tests required.
Laboratory staff must do the following:
- Confirm the applicant’s biodata and identity by comparing the photograph on the Laboratory Requisition and Report (IMM 5419), the photograph on the applicant’s approved identity document and the applicant reporting for laboratory tests.
- Document any identity concerns on the paper laboratory requisition forms. In such cases, laboratory testing may continue, and the panel physician will report the concerns to IRCC for follow-up.
- Fill out the declaration to confirm the following:
- the requested laboratory tests have been performed
- the sample for testing was collected from the client identified on the requisition
Urinalysis
A urinalysis is mandatory for all clients five years of age or older.
Refer to the Diabetes, hypertension, chronic renal or cardiac diseases TI for detailed recommendations on screening.
Syphilis serology
Syphilis is significantly prevalent in many regions of the world. You must pay special attention during the IME for all clients that have risk factors for syphilis, particularly those originating from areas with a high prevalence of syphilis.
Syphilis screening is required for all clients 15 years of age and older undergoing an IME. You must also request syphilis testing for clients below the age of 15 with any of the following risk factors:
- signs or symptoms compatible with syphilis infection
- high-risk sexual activity (for example, unprotected anal or vaginal sex, or multiple sexual partners)
- history of another sexually transmitted infection such as HIV, herpes, chlamydia, gonorrhea
- history of being born to a mother diagnosed with syphilis
- history of sexual contact with a known case of syphilis
- history of pregnancy
- for men, a history of having sex with other men
- history of sex work
- injection drug use
The evaluation consists of a medical history, physical examination and laboratory tests. You are required to report:
- if the applicant shows any signs or symptoms related to syphilis
- if the applicant has had a previous syphilis diagnosis
- evidence of recent or previous treatment
Symptoms are non-specific and it is entirely possible to go through the early stages of the infection without knowing about it.
See IRCC's technical instructions for more information – in particular, the syphilis TI.
If you see positive syphilis serology results from an applicant, you must:
- treat the syphilis according to the Canadian Guidelines on Sexually Transmitted Infections and provide proof of treatment
- accept previous treatment carried out according to the Canadian Guidelines on Sexually Transmitted Infections and provide proof of such treatment
IRCC requires the following treatment information:
- dates
- medications
- dosages
To prove that treatment has been provided to the applicant, you may either include proof of treatment information in the general supporting comments of the syphilis test section or attach a report to the IME.
HIV serology
HIV screening is required for all clients 15 years of age or older undergoing an IME. Panel physicians must also request HIV screening for clients below the age of 15 with any of the following risk factors (TB high-risk group, refer to TB TI):
- signs and/or symptoms compatible with HIV diagnosis
- history of being sexually active
- history of another sexually transmitted infection such as syphilis, herpes, chlamydia, gonorrhea
- history of sharing contaminated needles, syringes and other infected equipment and drug solutions for injection drug use
- history of receiving unsafe injections, blood product transfusions or medical procedures that involve unsterile cutting or piercing
- accidental needle stick injuries, including among health workers
- suspected active tuberculosis, hepatitis B, hepatitis C
- tattoos, body piercing, or acupuncture not thought to be done with aseptic technique
- history of being born to an HIV positive mother
- any child showing failure to thrive
You should also do the following:
- Provide the applicant with culturally sensitive, age and gender appropriate pre- and post-test counselling.
- Consider legal, ethical, social and human rights issues.
- If you use an interpreter, select one who is unbiased and has no connection to the applicant. Family members or friends cannot act as interpreters. The applicant must pay the cost of a professional interpreter.
- Provide pre-test counselling that includes information on the following:
- how HIV is transmitted and prevented
- a description of the testing procedure
- confidentiality of HIV testing, reporting and record handling
- the meaning of HIV screening test results, including the possibility of false positive or false negative results
- the need to inform anyone at risk of infection if the test is positive
- the applicant’s consent to undergo testing
You can find detailed information about how to manage pre- and post-test counselling in International Organization for Migration (IOM) Guide for HIV Counsellors: IOM HIV Counselling in the Context of Migration Health Assessment.
For all clients with positive HIV testing, panel physicians must provide a completed (signed and dated) IMM 5728: Acknowledgement of Post-test Counselling form, available in Appendix III.
Chest X-Ray Requisition and Report
Routine posterior-anterior chest x-rays (CXRs) are mandatory for applicants 11 years of age or older. A panel physician should request a CXR, regardless of age, if the medical questionnaire reveals a history of tuberculosis infection or treatment in applicants or their close contacts. All chest X-ray reports must be submitted along with a CD image in DICOM format. DICOM tag elements must state the client’s name, DOB, gender and the institution name.
The CXR must be examined for:
- general radiological findings
- evidence of active or inactive TB disease
Information to include on the CXR
The panel physician must enter the applicant’s personal information on the chest x-ray (CXR) requisition form:
- surname
- given name
- date of birth
- IME or UMI number (if applicable)
- the applicant’s photograph must be attached to the CXR requisition form
If an applicant is pregnant for the CXR
There may be cases where an applicant is not pregnant for the IME, but is pregnant for the x-ray examination. If an applicant is pregnant and elects to proceed with the CXR examination with adequate pelvic lead shielding, there are no changes to the CXR procedures.
If the client chooses to defer her CXR because of pregnancy:
- The radiology clinic must notify the panel physician that the CXR has been deferred.
- The panel physician may complete the IME, except for the CXR.
- The IME is submitted only once the post-partum CXR is returned to the panel physician.
- See the sample Instructions for Pregnant Client - X-Ray Deferred (IMM 5733) form in Appendix III.
If the applicant is undergoing an upfront medical examination, then the applicant must be given a copy of the form Upfront Medical Report – Client Biodata and Summary (IMM 1017B upfront) so they can submit it with their visa application before undergoing the post-partum CXR.
CXR indicating active tuberculosis
A panel radiologist who indicates suspected active TB in the client’s CXR must notify the panel physician immediately. The radiologist sends the CXR and report to the panel physician, and the panel physician then submits it to IRCC along with the results of your examination. As the panel physician, you must also do the following:
- Arrange immediately to have the applicant referred for a TB investigation.
- For confirmed, active TB cases, notify the public health authorities according to the country’s or region’s public health guidelines and directives.
- Ensure that the treatment provided to the applicant follows WHO recommendations and protocols (PDF, 1 MB).
For all confirmed active pulmonary TB cases, you must also:
- conduct screening for hepatitis B and C
- conduct screening for HIV (if not already done)
- proceed with contact screening for all family members or close contacts who are also IRCC clients
- recommend that non-IRCC close contacts see their own physicians for screening
- complete the IME and submit it to IRCC
As a result of contact tracing, applicants discovered to have latent TB should be reviewed by a local TB specialist to determine if treatment is recommended.
See IRCC's technical instructions for more information.
Radiology grading
Radiologists must provide a radiology grade based on their reported findings.
- Grade A indicates that there is no evidence of TB or abnormalities suggestive of other significant diseases identified.
- Grade B indicates that there is evidence of TB or abnormalities suggestive of other significant diseases identified.
- Comments should not be included for A-grade chest x-rays.
- Comments are mandatory for B-grade chest x-rays.
Panel Radiologist Declaration
Radiologist declarations are provided in writing on the radiology report and include the panel radiologist’s name, signature, number and the date of the CXR report.
Submitting CXRs
- The radiologist provides the general and special findings and grades the digital CXRs or film using the proper form.
- The radiologist or authorized radiology staff forward the CXRs and the report to the panel physician.
- The panel physician reviews the radiologist’s report and grading.
- Once all examinations are completed, the panel physician send the IME to IRCC.
Resettlement Needs Assessment (IMM 5544)
When an applicant is being processed as a refugee overseas, the migration office issues a Medical Report: Client Biodata and Summary (IMM 1017) with the IMM category of “refugee overseas”.
In such cases, the Resettlement Needs Assessment (IMM 5544) is included in the medical instructions sent to the applicant by a migration office as part of the IME.
As the panel physician, you must complete the Resettlement Needs Assessment IMM 5544 along with the IME and send them both.
Pregnant Client – X-Ray Deferred (IMM 5733)
If the client chooses to defer her Chest x-ray (CXR) because of pregnancy, the following steps apply:
- Complete the CXR requisition and give it to the applicant.
- Complete the Instructions for Pregnant Client – X-Ray Deferred (IMM 5733) and give it to the applicant. (The applicant may forward a copy of the IMM 5733 to the migration office as proof that the IME has been started and the CXR has been deferred because of pregnancy.)
- You may complete the IME, except for the CXR.
- Send the IME only once the post-partum CXR has been returned to you.
See the sample Instructions for Pregnant Client - X-Ray Deferred (IMM 5733) form in Appendix III.
If the applicant is undergoing an upfront medical examination, then the applicant must be given a copy of Upfront Medical Report – Client Biodata and Summary (IMM 1017B upfront) form for them to submit with their visa application prior to undergoing the post-partum CXR.
Additional Forms for paper-based IMEs
- IMM 5725: Activities of Daily Living (ADL)
- IMM 5738: Chart of Early Childhood Development (CECD)
- IMM 5728: Acknowledgment of HIV Post-Testing Counselling
- IMM 5734: Specialist’s Referral Form
- IMM 5738: Chart of Early Childhood Development (CECD)
Additional information for submitting forms
IME grading: Grade A or Grade B
Before you submit the IME, you must provide a grade for it based on your reported findings:
- Grade A indicates that there are no abnormal findings present and no significant abnormal history.
- Grade B indicates that there are significant abnormal findings present and/or an abnormal history.
- Comments cannot be included for A-grade IMEs.
- Comments are mandatory for B-grade IMEs.
Panel physician declaration
The panel physician’s declaration is provided in writing on the Medical Report (IMM 1017) and includes your name, signature, number and the date of the IME submission.
Furtherance process
RMOs may need more information to complete their medical assessment. They get this through the furtherance process. Furtherance might create additional costs for the applicant because the panel physician involved cannot be employed at the clinic where the initial IME was completed.
Here is what is involved in the furtherance process:
- The RMO issues a letter to the applicant with instructions to return to a panel physician for further investigations.
- The RMO provides the applicant with a sealed letter for the panel physician, which details the specific instructions for further investigations.
- As the panel physician, you either complete the additional examination(s) or refer the client to a specialist.
- Your referral letter must include the client’s biodata and photograph, and clearly indicate the investigations required by IRCC.
- Once all the required investigations have been completed, you return the reports to IRCC.
NOTE: If a furtherance is issued on paper it cannot be completed in eMedical.
Legislation related to the Immigration Medical Examination
Immigration is a shared federal/provincial responsibility. As a panel member, you should be aware of the following three pieces of legislation – in particular how they relate to the administration of IMEs, your responsibilities for protecting the personal information of applicants and how an applicant can be denied admission on health grounds.
The Immigration and Refugee Protection Act
The Immigration and Refugee Protection Act (IRPA) is a federal act. One of its objectives is to ensure that the movement of people into Canada contributes to the country’s cultural, social, and economic interests, and affirms its humanitarian commitments while protecting the health, safety and security of Canadians.
IRPA and its accompanying regulations set out the medical requirements for applicants who want to come to Canada as temporary or permanent residents. The legislation also sets out the grounds on which a person may be found to be inadmissible to Canada – including inadmissibility on health grounds.
A foreign national can be found inadmissible on health grounds if their medical condition:
- is likely to be a danger to public health
- is likely to be a danger to public safety
- might reasonably be expected to cause an excessive demand on health or social services
The Privacy Act
The purpose of this legislation is to protect the privacy of people’s personal information when it is collected, retained, used and disclosed by government, and provide individuals with the right to access their personal information.
Many aspects of the Privacy Act apply to your work as a panel member – in particular your responsibility to protect the information of the applicants you examine.
Take a closer look at the Privacy Act.
Collection of panel members’ personal information under IRPA
IRCC’s Migration Health Branch is responsible for administering the department’s medical screening program. This includes managing panel members who perform IMEs in Canada and abroad. As part of the medical screening program, the branch collects and creates personal information about panel members, including your:
- name
- business name
- provider type/specialty
- professional affiliation, licensing or certification
- contact information (address, postal code)
- languages spoken
- sex
- signature
- photograph
- evaluations performed by IRCC’s Migration Health Branch
- evaluations shared with Canada by the governments of Australia, New Zealand, the United Kingdom and the USA
The Access to Information Act
The Access to Information Act gives every Canadian citizen, permanent resident, individual or corporation in Canada the right to request access to records, in any format, held by a government institution, subject to certain exceptions.
Take a closer look at the Access to Information Act.
Find out how to request access to information or personal information.
It is not necessary for applicants to use these acts to get a copy of their own IME. As a panel physician, you are authorized to give them a copy if they ask.
Acronyms, Initialisms and Definitions
The following list provides definitions for acronyms and technical terms found in this guide:
- ADL:
- Activities of daily living
- Biodata:
- Information that establishes each client’s identity
- CECD:
- Chart of Early Childhood Development
- IRCC:
- Immigration, Refugees, and Citizenship Canada
- Chief radiologist:
- Licensed radiologist designated by IRCC to perform, grade and submit chest x-rays for Canada’s immigration medical examinations (IMEs).
- Client:
- A foreign national seeking to enter or remain in Canada who may be required to submit to an IME (in accordance with the Immigration and Refugee Protection Act and its regulations).
- Clinic staff:
- Persons who are working in the panel member’s clinic and may be involved in the immigration medical examination process.
- CXR:
- Chest x-ray
- ED:
- Excessive demand – a type of demand placed by a client on Canadian health or social services.
- EDE:
- Excessive demand exempt refers to specified groups of IRCC clients who are not denied entry or permission to stay in Canada because their medical condition may create an excessive demand.
- ELISA:
- Enzyme-linked immunosorbent assay, also known as enzyme immunoassay, which is one of the types of blood tests used to screen for HIV infection.
- eMedical:
- An online application that provides a paperless process for electronic recording, transmission and storage of immigration medical examination results.
- Furthered cases:
- Cases that require additional supplemental information.
- GAF:
- Global assessment of functioning
- Guardian:
- A person who looks after and is legally responsible for someone who is unable to manage their own affairs, especially an incompetent or disabled person or a child.
- Guide:
- This guide is the standard reference for the orientation and training of panel members. All panel members must ensure that they remain familiar with it and with related departmental instructions, including interim changes and updates provided by IRCC.
- HIV:
- Human immunodeficiency virus
- IFHP:
- Interim Federal Health Program – a program funded by IRCC that provides limited, temporary coverage of costs related to health screening and care for specific categories of people, including protected persons, refugee claimants (asylum seekers in Canada), rejected refugee claimants in Canada, certain persons detained under the Immigration and Refugee Protection Act and other specified groups.
- IGRA:
- Interferon gamma release assay. A blood test that is a screening test used to determine if a client has latent (inactive) tuberculosis.
- IMA:
- Immigration medical assessment – the medical opinion made by Migration Health Branch concerning an IRCC client’s health admissibility to Canada as defined under immigration legislation.
- IME:
- Immigration medical examination – the examination conducted by panel members. The results of these examinations are sent to IRCC regional medical offices via eMedical (or exceptionally by courier/post) who then provide an IMA.
- IME number:
- Immigration medical examination number – a unique number assigned to a specific IME.
- IMM 1017:
- An IME form containing the client’s biodata, IME grading and panel physician declaration.
- IMM 5419:
- An IME form containing the client’s medical history, physical examination findings, laboratory and the chest x-ray requisition results.
- IMM 5544:
- Supplemental medical and resettlement needs assessment form providing information on special accommodations a refugee may require to settle in Canada.
- IOM:
- The International Organization for Migration, an intergovernmental organization that became a related organization of the United Nations in 2016.
- IRCC:
- Immigration, Refugees, and Citizenship Canada. The Canadian federal government department that has primary responsibility for managing the entry into Canada of foreign nationals.
- IRPA and IRPR:
- Immigration and Refugee Protection Act and the Immigration and Refugee Protection Regulations (IRPR). Canadian legislation setting out the requirements for entry to Canada by foreign nationals. This legislation determines requirements to enter Canada including requirements for an IME. View the Act and regulations.
- LFT:
- Liver function test – a laboratory test used to evaluate liver function.
- locum tenens:
- Medical practitioners who replace panel physicians for a short period while they are on vacation, taking training or unable to provide service for other reasons.
- LTBI:
- Latent tuberculosis infection – sometimes referred to as ‘inactive tuberculosis’.
- Nominated radiologist:
- Licensed radiologist nominated by a chief radiologist located in the same radiology clinic to perform, grade and submit chest x-rays for Canada’s IMEs.
- Panel clinic:
- A clinic where designated physicians and/or radiologists conduct IMEs.
- Panel member:
- A general term that refers to a panel physician, panel radiologist or panel laboratories or specialists authorized by IRCC to perform IME related activities.
- Panel physician:
- A licensed medical doctor designated by IRCC to perform, grade and submit IMEs. Designated medical practitioner (DMP) was the previously used term.
- P number:
- A unique identifier given to specific panel members issued by IRCC’s Migration Health Branch.
- Protected person – In Canada:
- A person in Canada who according to Canada’s Immigration and Refugee Protection Act, is a person who has been determined to be either (a) a convention refugee or (b) a person in need of protection (including, for example, a person who is in danger of being tortured if deported from Canada).
- PTB:
- Pulmonary tuberculosis
- PTC:
- Post-test counselling
- Radiologist:
- For IRCC purposes, this refers to both chief and nominated radiologists.
- Refugee overseas:
- A person overseas who has been determined to be a convention refugee or a person in similar circumstances. A convention refugee is a person who meets the refugee definition in the Geneva Convention signed in 1951 relating to the status of refugees and the protocol to that convention signed in New York in 1967.
- RMO:
- RMO stands for regional medical office. These offices contain IRCC employees who are responsible for providing Canadian immigration medical services in a specific region. In 2019, there were four RMOs, located in Ottawa, London, New Delhi and Manila.
- TB:
- Tuberculosis.
- TIs:
- Technical instructions – the instructions for completion of the IME.
- TST:
- Tuberculin skin test. One screening test that can be used to determine if a person might have latent (inactive) tuberculosis infection.
- UCI:
- Unique client identifier. A unique number assigned to a client used for internal IRCC identification purposes.
- UFM:
- Upfront medical. An IME done prior to IRCC assigning a specific IME number to a client. Only certain IRCC clients can use UFM procedures.
- UMI:
- Unique medical identifier. A unique number used to associate to a specific upfront medical.
- VDRL:
- Venereal Disease Research Laboratory test, a blood test used to diagnose syphilis.
- Visa Officer:
- Any IRCC employee who under Canadian legislation has the delegated authority to make decisions/recommendations on visa issues. Previously the term visa officer referred to IRCC employees outside of Canada and migration officers referred to IRCC employees in Canada.
Section 3: Appendices
Appendix I: How to contact us
In Canada
For general inquiries about the Interim Federal Health Program (IFHP), please contact the IFHP team:
Migration Health Branch
Immigration, Refugees, Citizenship Canada
300 Slater Street, 7th Floor
Ottawa, ON K1A 1L1
Email: IRCC.IFHP-PFSI.IRCC@cic.gc.ca
To register as an Interim Federal Health Program service provider, and for inquiries about eligibility, benefits, claim requests or for general information, please contact the Medavie Blue Cross IFHP provider inquiry team:
IFHP Medavie Blue CrossTM
644 Main St., P.O. Box 6000
Moncton, NB E1C 0P9
Website: https://www.medaviebc.ca
Customer Service Centre: 1-888-614-1880
Email: CIC_Inquiry@medavie.bluecross.ca
Fax for inquiries: 506-867-4651
Fax for claims submissions: 506-867-3841
Send RMO Ottawa paper-based IME and other documents that cannot be uploaded to eMedical to:
Ottawa Regional Medical Office
Migration Health Branch
Immigration, Refugees, Citizenship Canada
300 Slater Street, 16th Floor
Ottawa, ON K1A 1L1
eMedical systems support
For service in English
Contact the Australian Department of Home Affairs via the “Contact Us” tab in the eMedical system.
For service in French
Email IRCC at: IRCC.MHBeMedical-eMedicalDGMS.IRCC@cic.gc.ca
This email is monitored from 8 a.m. to 4 p.m., Canadian Eastern Time, Monday to Friday, excluding statutory holidays.
For critical incidents
Contact IT support immediately.
Telephone: +61-2-6264-0400
Email: ITSupport@homeaffairs.gov.au
Critical incidents include the following:
- total loss of the eMedical system (unexpected outages)
- loss of core functions (cases cannot be submitted, attachments cannot be uploaded)
Note: This service is provided by the Australian Department of Home Affairs 24 hours a day, seven days a week, in English only.
For enquiries regarding medical clinical issues
Panel members should continue to direct all immigration medical exam-related enquiries to their regional medical office.
Regional medical offices
Your RMO is your point of contact for attaining your status as a panel member, submitting IME results and reports, and all other matters regarding your work as a panel physician or radiologist.
London
Overseas Regional Medical Office
Canadian High Commission
Canada House – Trafalgar Square
London SW1Y 5BJ
United Kingdom
Email: LDNPPMD@international.gc.ca
Manila
Overseas Regional Medical Office
Canadian Embassy
Level 7, Tower 2, RCBC Plaza
6819 Ayala Avenue
Makati City 0707
Philippines
Email: MANILMC-MD@international.gc.ca
New Delhi
Overseas Regional Medical Office
High Commission of Canada
7/8 Shantipath, Chanakyapuri
New Delhi 110021
India
Email: Delhimcdmp@international.gc.ca
Americas
Ottawa Regional Medical Office
Migration Health Branch
Immigration, Refugees, Citizenship Canada
300 Slater Street
Ottawa, ON Canada K1A 1L1
Email: IRCC.MHBRMOOttawa-OttawaBMRDGMS.IRCC@cic.gc.ca
Appendix II: Client Declaration and Notice (IMM 5743)




Appendix III: Forms
- IMM 1017: Medical Report – Client Biodata and Summary
- IMM 1017B upfront: Upfront Medical Report – Client Biodata and Summary
- IMM 5419: Medical Report
- IMM 5725: Activities of Daily Living (ADL)
- IMM 5728: Acknowledgment of HIV Post-Testing Counselling
- IMM 5733: Instructions for Pregnant Client - X-Ray Deferred
- IMM 5734: Specialist’s Referral Form
- IMM 5738: Chart of Early Childhood Development (CECD)
IMM 1017: Medical Report – Client Biodata and Summary

IMM 1017B upfront: Upfront Medical Report – Client Biodata and Summary


IMM 5419 Medical Report






IMM 5725: Activities of Daily Living (ADL)

IMM 5728: Acknowledgment of HIV Post-Testing Counselling

IMM 5733: Instructions for Pregnant Client - X-Ray Deferred

IMM 5734: Specialist’s Referral Form

IMM 5738: Chart of Early Childhood Development (CECD)



Appendix IV: List of immigration medical examination technical instructions
A) TIs related to process changes resulting from eMedical implementation
-
Activities of daily living (ADL)
Subject
Instructions for completing the Activities of Daily Living (ADL) form in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with a possible diminished ADL capacity
- Completion of the ADL form
- Completion and grading of an IME for a client with diminished ADL functions
Instructions
The ADL assessment provides information about which activities of daily living are impacted by disability due to mental or physical conditions/illnesses. PPs must evaluate clients’ activities of daily living and rate them accordingly. Scoring is based on their level of function, how independently a task can be performed, and whether supervision or assistance is needed in performing the task.
An ADL assessment is mandatory for all clients who:
- are 75 years of age or older
- have abnormal findings on physical examination of the musculoskeletal system
- have abnormal findings on physical examination of the nervous system
- have abnormal findings on physical examination suggestive of cognitive impairment or intellectual disability; and /or
- have an ongoing physical or mental health condition that might prevent them from attending a regular school program, obtaining full-time employment, or living independently
Reporting
PP’s must not refer clients to specialists unless instructed by the Regional Medical Office. All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME.
In parallel to the Immigration Medical Examination process, PPs are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
IMEs for clients with an abnormal ADL assessment must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s), submit the IME with a note indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: TI ADL (Activities of Daily Living)
TI ADL (Activities of Daily Living)
IME should be graded B if any abnormalities in the ADL assessment are found.
Q1: Is the client 75 years old or older?
No: No need for an ADL assessment
Yes: ADL assessment is mandatory
Q2: Is there abnormal findings on physical examination of the musculoskeletal system?
No: No need for an ADL assessment
Yes: ADL assessment is mandatory
Q3: Is there abnormal findings on physical examination of the nervous system?
No: No need for an ADL assessment
Yes: ADL assessment is mandatory
Q4: Is there abnormal findings on physical examination suggestive of cognitive impairment or intellectual disability?
No: No need for an ADL assessment
Yes: ADL assessment is mandatory
Q5: Is there an ongoing physical or mental health condition that might prevent the client from attending a regular school program, obtaining full-time employment, or living independently?
No: No need for an ADL assessment
Yes: ADL assessment is mandatory
-
Assessment of cognitive functioning
Subject
Instructions for assessing cognitive functioning in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with possible diminished cognitive capacity
- Completion and grading of an IME for a client with diminished cognitive capacity
Instructions
There are various tools available for assessing cognitive functioning (Mental State Exam, Montreal Cognitive Assessment). For the purpose of standardizing scores, the raw score of the tool used to assess cognitive functioning must be transposed to a scale of 30. In scoring the client’s cognitive functioning, the PPs may need to take into account mitigating factors such as the client’s educational attainment, literacy and cultural considerations. In certain circumstances, the raw score may be interpreted upon consideration of additional information such as anecdotal information from family members.
An assessment of cognitive functioning is mandatory for all adult clients who:
- are 75 years of age or older
- have abnormal findings on physical examination of the nervous system
- have abnormal findings on physical examination suggestive of cognitive impairment or intellectual disability; and/or
- have an ongoing physical or mental health condition that might prevent them from attending a regular school program, obtaining full-time employment, or living independently
Reporting
PP’s must not refer clients to specialists unless instructed by the Regional Medical Office. All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME.
In parallel to the Immigration Medical Examination process, PPs are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
All IMEs for clients with a cognitive functioning score of 25/30 or lower must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s), submit the IME with a note indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: TI for cognitive functioning assessment
TI for cognitive functioning assessment
IME should be graded B if any abnormalities in the cognitive functioning assessment are found.
Q1: Is the client 75 years old or older?
No: No need for a cognitive functioning assessment
Yes: cognitive functioning assessment is mandatory
Q2: Is there abnormal findings on physical examination of the nervous system?
No: No need for a cognitive functioning assessment
Yes: cognitive functioning assessment is mandatory
Q3: Is there abnormal findings on physical examination of the musculoskeletal system?
No: No need for a cognitive functioning assessment
Yes: cognitive functioning assessment is mandatory
Q4: Is there abnormal findings on physical examination suggestive of cognitive impairment or intellectual disability?
No: No need for a cognitive functioning assessment
Yes: cognitive functioning assessment is mandatory
Q5: An ongoing physical or mental health condition that might prevent the client from attending a regular school program, obtaining full-time employment, or living independently
No: No need for a cognitive functioning assessment
Yes: cognitive functioning assessment is mandatory
-
COVID-19 vaccines
Note: The following instructions are only for panel physicians practising outside of Canada.
The COVID-19 vaccine given at the time of the immigration medical examination (IME) is strictly voluntary, and clients must consent to receive the vaccine. Panel physicians are responsible for ensuring local requirements are followed when getting consent for vaccination.
Subject
Instructions for administering COVID-19 vaccines accepted by the Government of Canada or recording proof of COVID-19 vaccination at the time of the IME.
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) outside of Canada follow a consistent and appropriate process for the following:
- administering COVID-19 vaccines accepted by the Government of Canada
- recording proof of COVID-19 vaccination presented by clients
Background
In support of global efforts to reduce the transmission and spread of COVID-19, Immigration, Refugees and Citizenship Canada (IRCC) is encouraging all panel physicians to offer a COVID-19 vaccine accepted by the Government of Canada to their clients undergoing an IME, where available and accessible. IRCC will collect information related to the client’s COVID-19 vaccine history, including timing and type of vaccines received.
COVID-19 vaccines are not a mandatory component of the IME and will have no bearing on visa issuance or immigration admissibility to Canada, but PPs should offer the vaccine to clients during the IME, where available and accessible. The recording of vaccine history will provide IRCC with information about international access to COVID-19 vaccines accepted by the Government of Canada, general COVID-19 vaccine uptake, and other relevant trends that could be used to inform future program and policy decisions.
Instructions
Administering COVID-19 vaccines accepted by the Government of Canada
If available, PPs may administer any COVID-19 vaccine accepted by the Government of Canada. PPs must not wait to administer the subsequent dose(s) before submitting the IME, but should offer to administer or provide information about subsequent doses to clients where appropriate. Follow the guidelines in your jurisdiction regarding vaccine mixing.
Note: If clients require TST/IGRA testing during the IME as per the tuberculosis technical instructions, it should be performed before a vaccine is administered.
After administering any dose of a COVID-19 vaccine accepted by the Government of Canada to a client, take the following steps:
- Complete the 951 Vaccinations Exam to record the PP-administered vaccination. Consult the eMedical tip sheet instructions on where to enter PP-administered vaccines.
- Do not upload a copy of the vaccination record or any related documents.
- In the Remarks section in the 951 Vaccinations Exam, do not record information about client immunity or history of COVID-19 illness.
- After submitting the 951 Vaccinations Exam, give the client a copy of the Vaccination Worksheet for their records.
Recording proof of prior COVID-19 vaccination
PPs should instruct clients to provide all available records of COVID-19 vaccination for review, regardless of the number of doses received or the type(s) of vaccine received.
Acceptable vaccination documentation must come from a vaccination record, either a personal vaccination record or a copy of a medical chart with entries made by a physician or other appropriate medical professional. Follow your local public health guidance to determine whether the documentation provided is acceptable.
Vaccination records should include the vaccination received and date of administration. The document must not appear to have been altered, and dates of vaccinations should seem reasonable. Self-reported vaccine doses without documentation are not acceptable.
Use the 951 Vaccination Exam to record vaccination information for clients with proof of prior vaccination. Record the vaccination history for all types of COVID-19 vaccinations, regardless of whether the vaccines are accepted by the Government of Canada for border entry or quarantine exemptions.
- Review the client’s vaccination record.
- Complete the 951 Vaccinations Exam for any COVID-19 vaccine that the client has received, whether it be from the PP or from a prior source.
- In the Remarks section of the vaccine module, do not record any information about the client’s immunity or history of COVID-19.
- In the Attachments section in the 951 Vaccinations Exam screen, do not upload a copy of the vaccination record or any related documents.
Tips for completing the 951 Vaccinations Exam section
If the client has already received a COVID-19 vaccine, fill out the record results section for each COVID-19 vaccine the client has received by selecting the appropriate COVID-19 vaccine. Within the screen for recording the vaccine, fill out the appropriate sections and record whether
- the PP administered the vaccine or
- the vaccine was previously administered
If the PP does not administer a COVID-19 vaccine accepted by the Government of Canada at the time of the IME, select the relevant reason in the “Reasons for not providing vaccine” section.
If a client is already fully vaccinated before the IME, do not select one of the “Reasons for not providing vaccine”. IRCC will be able to determine if a client is fully vaccinated from an analysis of the vaccination history.
Do not upload a copy of the vaccination record or any related documents in the Attachments section.
For detailed instructions on how to complete the 951 Vaccinations Exam section for different scenarios, consult Appendix A and the algorithm.
Grading and submission of files
Clients with a COVID-19 vaccine do not require a B grading unless a B grading is indicated in conditions outlined in the Canadian Panel Member Guide to Immigration Medical Examinations.
Submit all files within the 10-day client service standard.
References
Information for clients:
Algorithm: Technical instructions for administering and recording COVID-19 vaccination in eMedical

Text version: Technical instructions for administering and recording COVID-19 vaccination in eMedical
Scenario 1 (Client already vaccinated):
Client provides proof of a previously obtained COVID-19 vaccine.
In the 951 Vaccinations Exam, select "COVID-19" in the drop-down list. Select the vaccine and record the vaccination data in the appropriate fields.
Complete the eMedical 951 Vaccinations Exam. Grade A and submit IME.
Scenario 2 (Vaccine unavailable):
In the 951 Vaccinations Exam, select "COVID-19" in the drop-down list. In the "Disease level questions" section, select "No vaccines for this disease are currently available at the Panel Site" under the "Reasons for not providing the vaccine".
Complete the eMedical 951 Vaccinations Exam. Grade A and submit IME.
Scenario 3 (Vaccine is administered): The Panel clinic has stock of COVID-19 vaccines accepted by the Government of Canada and can offer the vaccine to the client at the time of the IME.
Vaccine is administered. In the 951 Vaccinations Exam, select "COVID-19" in the drop-down list. Select the vaccine and record the vaccination data in the appropriate fields.
Complete the eMedical 951 Vaccinations Exam. Grade A and submit IME.
Scenario 4a (Client denies vaccination):
In the 951 Vaccinations Exam, select "COVID-19" in the drop-down list. In the "Disease level questions" section, select "Applicant declined all vaccines for this disease" under the "Reasons for not providing the vaccine".
Complete the eMedical 951 Vaccinations Exam. Grade A and submit IME.
Scenario 4b (vaccination not administered for other reasons):
In the 951 Vaccinations Exam, select "COVID-19" in the drop-down list. Select the type of vaccine(s) offered in the drop-down list and record reason for not providing the vaccine.
Complete the eMedical 951 Vaccinations Exam. Grade A and submit IME.
Appendix A: How to complete the 951 Vaccinations Exam section for different scenarios
Scenario Situation Disease level questions Vaccine type Vaccination history
* After documentation provided voluntarily by the client is reviewed and verified.Vaccination given by Panel Site Batch/Lot Reason for not providing vaccine Contraindications Remarks
* Do not record information about client being fully vaccinated, client immunity or history of COVID-19 illness.1 Vaccination not offered to client because client is already fully vaccinated, regardless of vaccine type. Not applicable Select the type of vaccine(s) in the COVID-19 drop-down list. Enter the date(s) of previously administered vaccine(s). Not applicable Not applicable Not applicable Not applicable Not applicable 2 No availability of a Government of Canada-accepted COVID-19 vaccine; no vaccine is offered to client. Select "No vaccines for this disease are currently available at the Panel site" If a prior dose of a COVID-19 vaccine was administered, select the type of vaccine(s) in the COVID-19 drop-down list. If a prior COVID-19 vaccine was administered, enter the date(s), including - past doses and
- future scheduled doses
Not applicable Not applicable Not applicable Not applicable Not applicable 3 Client consents to receive a Government of Canada-accepted COVID-19 vaccine and may provide a proof of prior vaccines, regardless of vaccine type. Not applicable Select the type of vaccine(s) in the COVID-19 drop-down list, including the one PP administers and the previous one. Enter the date(s) of previously administered vaccine(s). Enter the date(s) when you administered the vaccine. Record batch and lot number. Not applicable Not applicable Not applicable 4 Client provides proof of prior Government of Canada-accepted vaccines.
Note: PP must review proof and make a determination on whether proof is sufficient, based on in-country procedures or guidelines or the PP’s own expertise.
Select an option, if applicable Select the type of vaccine(s) in the COVID-19 drop-down list. Enter the date(s) of previously administered vaccine(s). Not applicable Not applicable Not applicable Not applicable Not applicable 5 Client provides proof of prior non-Government of Canada-accepted vaccines.
Note: PP must review proof and make a determination on whether proof is sufficient based on in-country procedures or guidelines or the PP’s own expertise.
Select an option, if applicable Select the type of vaccine(s) in the COVID-19 drop-down list. If the type of vaccine is not listed, enter the vaccine type(s) under Other (COVID-19) 1. Enter the date(s) of previously administered vaccine(s). Not applicable Not applicable Not applicable Not applicable Not applicable 6 Client consented to receive the vaccine but an underlying medical condition found during the medical examination prevents PP from administering the vaccine. Not applicable If a prior dose of a COVID-19 vaccine was administered, select the type of vaccine(s) in the COVID-19 drop-down list. If a prior COVID-19 vaccine was administered, enter the date(s). Not applicable Not applicable Not applicable Select the appropriate contraindication. Not applicable 7 Client does not consent to receive the vaccine. Client may provide proof of prior vaccines, regardless of vaccine type. Select "Applicant declined all vaccines for this disease" If a prior dose of a COVID-19 vaccine was administered, select the type of vaccine(s) in the COVID-19 drop-down list. If a prior COVID-19 vaccine was administered, enter the date(s). Not applicable Not applicable Not applicable Not applicable Not applicable -
Vaccination
Note: The following instructions are only for panel physicians practicing outside of Canada.
Note: PPs registered with the Interim Federal Health Program (IFHP) Pre-Departure Medical Services (PDMS) must follow the vaccination instructions, schedule and documentation form included in the IFHP Immunization Manual (PDF, 1.5 MB).
Vaccination at the time of the immigration medical examination (IME) is strictly voluntary, but clients who choose to be vaccinated must provide consent to receive vaccines and to disclose their vaccine information to Immigration, Refugees and Citizenship (IRCC). Panel physicians (PPs) are responsible for ensuring local requirements are followed when obtaining free and informed consent for vaccination.
Subject
Instructions for administering vaccinations and recording proof of vaccination at the time of the IME.
Goal/objective
These instructions are provided to ensure that PPs outside of Canada follow a consistent and appropriate process for the following:
- administering vaccines for vaccine-preventable diseases (VPDs)
- recording proof of vaccination presented by clients
- providing clients with a print out record of vaccinations
Background
In support of global efforts to reduce the transmission and spread of vaccine preventable diseases, IRCC is encouraging all PPs to assess the vaccination status of clients and, with consent, offer vaccines where available and accessible. IRCC will collect information related to the client’s vaccine history, including timing and type of vaccines received where clients have provided consent.
Vaccination is not a mandatory component of the IME and will have no bearing on visa issuance or immigration admissibility to Canada.
COVID-19 vaccines may continue to be offered to clients on a voluntary basis at the time of the IME in addition to other vaccines described here as part of this new initiative. For further information, please see the COVID-19 Technical Instructions.
Instructions
Recording proof of prior vaccination
PPs should seek client consent to disclose vaccine information to IRCC and request that clients provide all available records of vaccinations for review.
Acceptable vaccination documentation must come from a vaccination record, either a personal vaccination record or a copy of a medical chart with entries made by a physician or other appropriate medical professional. Follow your local guidelines to determine whether the documentation provided is acceptable.
Vaccination records should include the vaccination received and date of administration. The document must not appear to have been altered, and dates of vaccinations should seem reasonable. Self-reported vaccine doses without documentation are not acceptable. Laboratory confirmation of immunity and history of disease are not required and must not be recorded in the 951 Vaccination Exam.
Use the 951 Vaccinations Exam to record vaccination information for clients with proof of prior vaccination. Record the vaccination history for all types of vaccinations, regardless of whether the vaccines are part of a catch-up schedule.
- Seek consent from the client to disclose their vaccination record, and review the client’s vaccination record.
- Complete the 951 Vaccinations Exam for any vaccine that the client has received, whether it be from the PP or from a prior source.
- Do not upload a copy of the vaccination record or any related documents. Vaccine status related information as well as any information regarding vaccines administered during the IME must never be attached to IMEs or entered in the notes.
- In the Remarks section in the 951 Vaccinations Exam, do not record any information about the client.
- Provide the client with a copy of the Vaccination Worksheet for their records.
Administering vaccines for VPDs
Note: If clients require TST/IGRA testing during the IME as per the tuberculosis technical instructions, it should be performed before a vaccine is administered.
IRCC will not supply or cover costs related to vaccines administered by PPs outside of PDMS. If available, PPs may administer vaccines to clients against any of the following diseases:
- measles
- mumps
- rubella
- diphtheria
- tetanus
- pertussis
- haemophilus influenza b
- hepatitis B
- rotavirus
- poliovirus
PPs must assess the client’s suitability to receive vaccinations in accordance with local guidelines.
For clients without records of previous vaccination or for those not previously vaccinated, or inadequately vaccinated, vaccines should be offered in accordance with local guidelines.
For multi-dose series, PPs must not wait to administer a subsequent dose(s) before submitting the IME, and should initiate the series and provide information to the client about subsequent doses required and the timing of these. PPs may refer to the Canadian Immunization Guide for recommended immunization schedules.
PPs must be prepared to manage acute adverse events following immunization, such as anaphylaxis, in accordance with local guidelines.
Note: PPs should seek client consent to disclose any information related to vaccines received at the Panel Site to IRCC. Vaccine-related information includes type of vaccination(s) received, date(s) of vaccination and/or reason a vaccination was not offered and/or not administered.
Use the 951 Vaccinations Exam to record vaccination information for clients who receive a PP-administered vaccine:
- Seek consent from the client to receive the vaccine and administer vaccine.
- Seek consent from the client to record and disclose any information related to vaccines received at the Panel Site to IRCC. If you do not obtain consent, do not record any information.
- Complete the 951 Vaccinations Exam to record the PP-administered vaccination, including:
- Date of administration
- Vaccine type
- Batch/lot
- Any contraindications, if applicable.
- Consult the eMedical tip sheet on where to enter PP-administered vaccines.
- Complete the 951 Vaccinations Exam to record the PP-administered vaccination, including:
- Do not upload a copy of the vaccination record or any related documents. Vaccine status related information as well as any information regarding vaccines administered during the IME must never be attached to IMEs or entered in the notes.
- In the Remarks section in the 951 Vaccinations Exam, do not record any information about the client.
- After submitting the 951 Vaccinations Exam, give the client a copy of the Vaccination Worksheet for their records.
If you are a registered provider with the IFHP and are administering vaccines to refugees as part of PDMS:
- Do not complete the 951 Vaccinations Exam module to record PP-administered vaccination.
- Please document vaccine history and any doses given to the client in the PDMS Vaccination Documentation Worksheet.
- For current copies of the Vaccination Documentation Form and PDMS Vaccination Manual please visit IFHP PDMS website at https://www.medaviebc.ca/en/health-professionals/pre-departure-medical-services.
Tips for completing the 951 Vaccinations Exam section
The PP must only record information within the 951 Vaccination Exam section if the client has provided consent to disclose this information to IRCC.
If the PP does not administer any vaccines at the time of the IME and the client consents to their information being disclosed to IRCC, select the relevant reason in the “Reasons for not providing vaccine” section under the Disease Level Questions. If a client is already fully vaccinated before the IME, do not select one of the “Reasons for not providing vaccine”.
For detailed instructions on how to complete the 951 Vaccinations Exam section for different scenarios, consult Appendix A and the algorithm.
Grading and submission of files
Clients disclosing and receiving vaccines do not require a B grading unless a B grading is indicated in conditions outlined in the Canadian Panel Member Guide to Immigration Medical Examinations.
Submit all files within the 10-day client service standard.
References
Information for clients:
- Get Immunized - Canada.ca
- Vaccine-Preventable Diseases - Canada.ca
- Vaccines and immunization - Canada.ca
Frequently Asked Questions: Vaccination Pilot
I. General Information
What is the purpose of the vaccination pilot?
The objective of the pilot is to promote the increase of vaccination coverage rates among Canada bound migrants prior to traveling and to encourage them to carry their vaccination documentation for when they arrive in Canada.
Is it mandatory for clients undergoing an IME to participate in the pilot?
No, this initiative is not mandatory. It is completely voluntary for PPs and for clients.
Which panel sites can participate in the vaccination pilot?
Only panel sites in the overseas setting are taking part in the vaccination pilot. The objective is to promote the increase of vaccination coverage rates among Canada-bound migrants prior to traveling and to encourage them to carry their vaccination documentation for when they arrive in Canada.
What if clients do not participate?
The vaccination pilot that is underway is to inform the feasibility of a voluntary, expanded vaccination program. Therefore, proof of vaccination is not mandatory and is not required to complete the medical exam. However if the client has provided consent to share their vaccination history, it can be entered in eMedical even if they choose not to be vaccinated at the panel site. As the objective is to increase vaccination coverage of all Canada-bound migrants identified as under-immunized, we encourage participation where possible. Clients can also benefit from the protection against vaccine-preventable diseases of public health concern. Information collected during the pilot (e.g. vaccination uptake) and from surveying PPs will help guide next steps when this trial is completed.
What information will IRCC be collecting and what is the purpose of this information collection?
IRCC will collect information entered by the panel physician regarding a client’s vaccination history, any vaccines received at the panel site and any contraindications or reasons the client did not receive a vaccine (when client consent has been received for each component). The vaccine-related information collected during the pilot will inform the outcome and the next steps to advancing the Immunization Strategy, including the determination of whether IRCC will begin a vaccination program for migrants overseas where all clients will have the ability to voluntarily receive vaccines against vaccine preventable diseases.
Will this impact a client’s immigration application or the client’s IME results?
No, this vaccination pilot has no effect on a client’s immigration application nor on their IME results.
If participation in the vaccination pilot is not mandatory, what type of counseling can we offer?
We encourage PPs to offer counselling that is suited for each IRCC client. However, you may consider discussing the following points:
- It is a public health approach to support global health efforts to reduce the transmission and spread of vaccine preventable diseases
- It is the most effective preventive measure to protect against vaccine preventable diseases
- Sharing client vaccination information with Provinces and Territories can help prevent re-vaccination, and facilitate linkages with the health care system
II. Client Consent
What type of consent is required if a client decides to participate in the pilot?
Consent must be obtained from the client to:
- Record any previous vaccinations
- Administer vaccines at the Panel Site
- Record vaccines administered at the Panel Site
This is done by:
- Obtaining the client’s signature on form IMM5743 (the Client Declaration And Notice with Respect to the Immigration Medical Exam and Notice with Respect to Vaccination)
- Obtaining expressed and informed oral consent from the client before recording anything in the 951 module and before administering any vaccination
Any other established procedures for obtaining client consent in your region or jurisdiction are also acceptable.
III. Vaccination Records
What is acceptable proof of vaccination?
Acceptable vaccination documentation must come from a vaccination record, either a personal vaccination record or a copy of a medical chart with entries made by a physician or other appropriate medical professional. We request that you follow your local guidelines and use due diligence to determine whether the documentation provided is acceptable.
Do records need to be translated?
No, if medical records are in a language you do not speak nor understand, do not record any information. It is not necessary to have these documents translated.
Should I record vaccine doses directly reported by the client?
No, do not record any self-reported vaccine doses without documentation demonstrating proof of vaccination.
IV. Vaccine Procurement
Who is providing the vaccines for this pilot?
PPs who choose to participate must obtain vaccines as per availability and regulations in their respective local jurisdiction.
V. Vaccine Costs
Who will pay for the vaccines?
The clients pay for the vaccines they choose to receive, unless otherwise covered by a public entity or institution in their jurisdiction. On IRCC’s public facing websites, there is information informing clients of the opportunity to update their vaccination status at the Panel Site with an associated cost. However, as this pilot is still new, it is possible that clients are not yet aware. Please ensure clients are informed prior to administering any vaccines. We also ask, as per the Panel Physician Guide, that all immigration medical services charged to the client represent fairly the services you perform, and comply with local guidelines, or those of a medical association or group.
Are vaccines free in Canada?
Canada doesn’t have a single national plan; rather, each of our 13 separate provinces and territories have their own separate health care insurance plans. Provincial and territorial plans pay for basic healthcare and dental services and needs, however what’s covered will vary depending on where the client resides and their respective eligibility criteria. Each province and territory determines its own minimum requirements with regard to an individual's eligibility for benefits under its health insurance plan. In most cases, vaccines that are part of a provincial or territorial publicly-funded program are covered for its residents as long as they fulfill the jurisdiction’s eligibility requirements (e.g. minimum residence requirement).
If a question is raised by clients on provincial health coverage plans in Canada, we recommend PPs direct them to official Government of Canada websites, addressed to the public, which describes Health Care in Canada and general information on vaccines and immunization in Canada.
VI. Vaccine Administration
What vaccine types can we offer to clients?
IRCC is asking PPs to offer WHO or UNICEF approved vaccines. A list of vaccine types and antigens is available in eMedical for PPs to refer to. It is located under the eMedical Canada Specific folder listed under eMedical vaccination program for migrants.
Can we verify antibody titers to verify for immunity prior to vaccination? De we need to record history of disease or confirmation of immunity in eMedical?
We do not require laboratory confirmation of immunity nor history of disease to be performed and we ask that this information not be recorded in the 951 Vaccination Exam Module for the vaccination pilot. When assessing the clients suitability to receive vaccination the PP should follow the local guidelines of their jurisdiction. If the PP has received informed consent and the client does not have any documentation of previous vaccination or if the client is not previously vaccinated, the PP should follow their local guidelines to determine the appropriate approach.
What about the possibility of adverse effects following immunization?
We advise PPs who will offer vaccination to clients to be prepared to manage acute adverse events following immunization, such as anaphylaxis, in accordance with their respective local guidelines.
Can we direct clients to get vaccinated by a third-party provider?
If a PP is unable to provide vaccination at their clinic, it is encouraged for clients to be vaccinated by a third-party provider as per the local guidelines. However, as vaccination is not a required component of the IME, we advise PPs not to delay the client’s IME nor the submission of the IME file to await third-party vaccine documentation. You may wish to inform clients to bring their proof of vaccination for the IME appointment at the time of the appointment booking in order to better assess their vaccination status and make the appropriate vaccine recommendations to the client.
Will IRCC provide a vaccination schedule?
IRCC will not be providing a vaccination schedule for this pilot. If offering vaccines, PPs must assess the suitability for clients of all ages to receive vaccinations in accordance with their respective local guidelines.
If available, PPs may administer vaccines to clients against any of the following diseases: measles, mumps, rubella, diphtheria, tetanus, pertussis, haemophilus influenza type b, hepatitis B, rotavirus, and poliovirus.
Understanding that immunization schedules and vaccines may differ from those in Canada, we ask that PPs follow the immunization schedules in accordance to their respective local guidelines.
Algorithm: Technical instructions for recording and administering vaccination in eMedical

Text version: Technical instructions for recording and administering vaccination in eMedical
Determine your clinic’s vaccine stock. If the clinic does not have stock, click the checkbox for “No vaccines for the disease are currently available at the Panel Site” under the “Disease level questions” section of the module.
Seek consent from the client to record and disclose their previous immunization information to IRCC. If the client consents, record the client’s prior immunization data in the 951 Vaccine module. If the client does not consent, do not record anything.
You are then asked to assess the clients vaccination needs. If the client cannot be vaccinated at the Panel Site, inform the patient and seek their consent to record and disclose to IRCC the reason in the module (such as age, insufficient time during the appointment, contraindications etc.) If the client does not consent, do not record anything.
If the client can be vaccinated, obtain consent to administer a vaccine. If the client consents, administer the vaccine.
If you administer a vaccine at the Panel Site, seek consent from the client to record and disclose this vaccination to IRCC. If the client consents, record the information in the module (i.e. the vaccine type and the batch and lot numbers). If the client does not consent, do not record anything.
If you recorded any vaccination information, provide the client with a copy of their vaccination worksheet.
In all cases, grade and complete the 951 exam.
Appendix A: How to complete the 951 module for different scenarios
(For all scenarios, do not record and disclose any information if the client has not consented to disclose their vaccination information).
Scenario Situation Disease level questions Vaccine type Vaccination history (i.e. Non-Panel site) Other, specify if vaccine type not listed Vaccination at Panel Site Vaccination at Panel site, Batch/Lot Vaccination at Panel site, Reason for not providing vaccine Vaccination at Panel site, Contraindications Remarks
* Do not record information about client being fully vaccinated, client immunity or history of illness.1 Client is fully vaccinated. Client consents to disclosing vaccination history to IRCC. Select an option, if applicable. Select the type of vaccine(s) recorded on the vaccination history documentation. Enter the date(s) of previously administered vaccine(s). If a previously-administered vaccine is not listed in the drop down list, record the specific type of vaccine in this field. Otherwise, do not record anything. Do not record anything. Do not record anything. Do not record anything. Do not record anything. Do not record anything. 2 No vaccine is offered to the client due to lack of availability. Client consents to disclosing vaccination history to IRCC. Select “No vaccines for this disease are currently available at the Panel Site”. If a prior dose of a vaccine was administered, select the type of vaccine(s) recorded on the vaccination history documentation. If a prior dose of a vaccine was administered, enter the date(s) of relevant previously administered vaccine(s). If a previously-administered vaccine is not listed in the drop down list, record the specific type of vaccine in this field. Otherwise, do not record anything. Do not record anything. Do not record anything. Do not record anything. Do not record anything. Do not record anything. 3 Client is unvaccinated and consents to receiving vaccinations available to the PP against the VPD. Client consents to disclose this information to IRCC (no vaccination history to record). Do not record anything. Do not record anything. Do not record anything. Do not record anything. Enter the date(s) when you administered the vaccine. Record batch and lot number. Do not record anything. Do not record anything. Do not record anything. 4 Client is partially vaccinated and consents to get another dose. Client consents to disclose this information to IRCC. Client consents to disclosing vaccination history to IRCC. Do not record anything. Select the type of vaccine(s) recorded on the vaccination history documentation. Enter the date(s) of relevant previously administered vaccine(s). If a previously-administered vaccine is not listed in the drop down list, record the specific type of vaccine in this field. Otherwise, do not record anything. Enter the date(s) when you administered the vaccine. Record batch and lot number. Do not record anything. Do not record anything. Do not record anything. 5 Client is partially vaccinated with vaccines not listed in the module and consents to a further dose. Client consents to disclose this information to IRCC. Client consents to disclosing vaccination history to IRCC. Do not record anything. Select the type of vaccine(s) recorded on the vaccination history documentation that apply. Enter the date(s) of previously administered vaccine(s). If a previously-administered vaccine is not listed in the drop down list, record the specific type of vaccine in this field. Otherwise, do not record anything. Enter the date(s) when you administered the vaccine. Record batch and lot number. Do not record anything. Do not record anything. Do not record anything. 6 Client provides consent to receive the vaccine, but an underlying medical condition found during the medical examination prevents the PP from administering the vaccine. Client consents to disclose this information to IRCC. Client consents to disclosing vaccination history to IRCC. Do not record anything. Select the type of vaccine(s) recorded on the vaccination history documentation. Enter the date(s) of previously administered vaccine(s). If a previously-administered vaccine is not listed in the drop down list, record the specific type of vaccine in this field. Otherwise, do not record anything. Do not record anything. Do not record anything. Do not record anything. Select the appropriate contraindication. If the contraindication is not listed, select other. Do not enter any further information. Do not record anything. 7 Client does not consent to receive the vaccine against the VPD. Client consents to disclose this information to IRCC. Client consents to disclosing vaccination history to IRCC. Select “Applicant declined all vaccines for this disease”. Select the type of vaccine(s) recorded on the vaccination history documentation. Enter the date(s) of previously administered vaccine(s). If a previously-administered vaccine is not listed in the drop down list, record the specific type of vaccine in this field. Otherwise, do not record anything. Do not record anything. Do not record anything. Do not record anything. Do not select anything. Do not record anything. 8 Client does not consent to disclosing their vaccination history to IRCC. Client does not consent to disclosing any information on vaccines received at the Panel Site to IRCC. Select an option, if applicable. Do not record anything. Do not record anything. Do not record anything. Do not record anything. Do not record anything. Do not record anything. Do not record anything. Do not record anything. -
Developmental milestones: Chart of early childhood development
Subject
Instructions for evaluating early childhood development and completing the Chart of Early Childhood Development (CECD) section in the context of the Canadian immigration medical examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Assessment of developmental milestones for an infant or child
- Identification of infants /children with delayed developmental milestones
- Completion of section 904-CECD and reporting in eMedical
- Grading of an IME for a client with delayed developmental milestones and an abnormal CECD
Instructions
PPs are required to assess the developmental age for all children less than 5 years of age and complete section 904 in eMedical. PPs have to report the developmental age of the child:
- Observed by the client’s parents /caregivers
- Observed by himself during the IME
The CECD will assist PPs in their assessment of the developmental milestones. The CECD is a screening tool used to evaluate a child’s motor /physical, communication /language, social /emotional, and cognitive development from birth to 5 years of age.
Chart of early childhood development (CECD)
By 1 month of age
- Looks at parent /caregiver (focuses gaze)
- Calms when comforted
- Startles to loud or sudden noises
- Sucks well on nipple
By 2 months of age
- Follows movement with eyes
- Makes a variety of sounds (coos, gurgling)
- Lifts head up while lying on tummy
- Recognizes and calms to a familiar gentle voice
- Smiles responsively
- Has different cries (for example, when tired vs hungry)
- Holds head up when held at caregiver’s shoulder
By 4 months of age
- Follows a moving toy or person with eyes
- Holds head steady when supported at the chest or waist in a sitting position
- Responds to parent /caregiver by making sounds, moving limbs
- Glances from one object to another
- Holds an object briefly when placed in hand
- Laughs and smiles responsively
By 6 months of age
- Turns head and looks in direction of a new sound
- Rolls from back to side
- Uses hands to reach, grasp, bang, and splash
- Vocalizes pleasure and displeasure
- Makes sounds while parent /caregiver is talking to him /her
- Sits with support (for example, pillows)
- Brings hands or toy to mouth
By 9 months of age
- Looks for a hidden toy/object
- Stands with support when helped into standing position
- Sits without support for a few minutes
- Plays social games with parent/caregiver (for example, peak-a-boo)
- Babbles a series of different sounds
- Picks up small items using thumb and first finger
- Makes sounds/gestures to get attention or help
By 12 months of age
- Consistently uses 3 or more words (words do not have to be clear)
- Combines sounds together as though talking
- Pulls up to stand at furniture
- Picks up small items using tips of thumb and first finger
- Responds to own name (looks at person)
- Understands simple requests (for example “find your shoes”)
- Walks holding onto furniture or parent /caregiver’s hands
- Takes things out of containers (for example blocks)
By 15 months of age
- Consistently uses 5 or more words (words do not have to be clear)
- Walks sideways holding onto furniture
- Stacks 2 blocks
- Responds to own name when called
- Imitates a few animal sounds
- Crawls up a few stairs /steps
- Tries to squat to pick up a toy from the floor
- Shows fear of strange people /places
By 18 months of age
- Consistently uses 15 or more words (words do not have to be clear)
- Walks independently
- Stacks 3 or more blocks
- Shows affection towards people, pets, or toys
- Points to what he /she wants or to show parent /caregiver something
- Walks up a few stairs holding parent /caregiver’s hand
- Points to at least 3 different body parts when asked
By 24 months of age
- Combines 2 or more words
- Walks backward 2 steps without support
- Stacks 4 or more blocks
- Uses toys for pretend play (for example, give doll a drink)
- Understands 1 and 2 step directions/instructions
- Tries to run
- Puts objects into a small container
By 30 months of age
- Combines 3 or more words
- Uses pronouns such as I, you, me, and mine
- Jumps off the floor with both feet
- Tries to join in songs and rhymes with parent /caregiver
- Names most common items (for example, dog, apple, car)
- Runs without falling most of the time
- Kicks a ball forward
By 3 years of age
- Uses sentences with 5 or more words
- Understands 2 and 3 step directions /instructions
- Walks upstairs using handrail
- Turns pages of a book one at a time
- Plays with others comfortably
- Speaks clearly enough to be understood by family all of the time
- Listens to music or stories for 5-10 minutes
- Twists lids off jars or turns knobs
- Plays make-believe games with actions and words (for example, pretending to cook a meal)
- Shares some of the time
By 4 years of age
- Understands 3 step directions/instructions
- Tells stories with a clear beginning, middle, and end
- Walks up/down stairs with alternating feet
- Undoes buttons and zippers
- Uses toilet/potty during daytime
- Asks and answers lots of questions
- Identifies or shows you 4 colours when asked
- Stands on one foot for 1-3 seconds without support
- Draws a person with 3 or more body parts
- Tries to comfort someone who is upset
By 5 years of age
- Counts out loud or on fingers to answer “how many are there?”
- Speaks clearly in adult-like sentences most of the time
- Stops, starts, and changes direction smoothly when running
- Throws and catches a ball successfully most of the time
- Usually plays well in groups
- Works alone at an activity for 20-30 minutes
- Knows common shapes and most of the letters of the alphabet
- Tells long stories about own past experiences
- Hops on one foot several times
- Holds a crayon or pencil correctly
- Shares willingly with others
- Cooperates with adult requests most of the time
Reporting
For children where the observed developmental milestones are not consistent with the chronological age, the PP should provide all relevant information to clarify /confirm a diagnosis, identify medical and/or social services requirements (for example, medical services at home, special education, occupational therapy, speech language therapy, physiotherapy), and establish a prognosis over the next 5-10 years. This will help the medical officer make the determination of current and future (within the next 5-10 years) medical care and social service requirements of the child.
PP’s must not refer clients to specialists unless instructed by the Regional Medical Office (RMO). All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME.
In parallel to the immigration medical examination process, PPs are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
All IMEs for clients with abnormal developmental milestones must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s) submit the IME with a note indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: TI for Developmental Milestones
TI for Developmental Milestones
IME should be graded B if any developmental milestones are not consistent with the client’s chronological age and developmental delay is suspected. IME should be submitted including any existing test results and specialist reports.
Q1: Is the client 5 years old or less?
Yes: Complete an assessment of developmental milestones – Chart of Early Childhood Development
No: No need to proceed with an assessment of developmental milestones.
Q2: If an assessment of developmental milestones was performed, is the developmental milestones not consistent with the client’s chronological age and developmental delay is suspected?
Yes: Provide all relevant information to clarify /confirm a diagnosis, identify medical and/or social services requirements (e.g. medical services at home, special education, occupational therapy, speech language therapy, physiotherapy..), and establish a prognosis over the next 5-10 years.
Clients should not be referred to specialists unless instructed by the RMO.
No: Continue the medical examination.
References
-
Resettlement needs assessment
Subject
Instructions for evaluating and reporting the resettlement needs of refugees overseas who have been selected for resettlement in Canada in the context of the Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure panel physicians (PPs) follow a consistent and appropriate process in the:
- assessment of the resettlement needs of refugees overseas
- proper completion of the section 948 resettlement needs
Instructions
Background
It is important that refugees with extensive medical and/or social needs are able to 1) travel to Canada efficiently and safely and 2) be able to settle into Canada with their medical and social needs being recognized and attended to quickly and effectively.
The section 948 in eMedical; resettlement needs has been created in order to capture vital information in support of proper resettlement from a medical perspective. For all overseas refugees selected for resettlement in Canada, section 948 in eMedical is mandatory. In countries where eMedical is not implemented, the Visa Office will issue the IMM 5544 form “Resettlement needs Assessment Form” together with the medical instructions. (IMM 1017 Medical report: client biodata and summary).
The table below provides information for the PP regarding eMedical and paper-based submission of the IMM 5544.
eMedical-enabled panel clinics
- Visa Office (VO) issues IMM 1017 with IMM category of refugee-overseas
- Section 948 is required to be filled out in eMedical and submitted along with the health case
- IMM 5544
Paper-based panel clinics
- Visa Office (VO) issues IMM 1017 with IMM category of refugee-overseas
- IMM 5544 is included in medical instructions sent to client by VO as part of the IME
- Panel physician will complete the IMM 5544 and submit it along with the paper-based IME
The resettlement needs section is used to provide additional information for three important purposes:
- to facilitate safe and efficient travel to Canada
- to maximize post-arrival settlement arrangements on arrival to Canada
- and to help in determining the destination city in Canada where the medical and social services required for the refugee are available
Completing the resettlement needs section
The Resettlement needs section is to be completed for every overseas refugee, even those without medical conditions or concern. Even a negative answer is important. When a refugee has no special travel requirements or settlement issues, the PPs must check the box following the statement “There are no special travel requirements or resettlement needs” (see figure below):

Text version
There are no special travel requirements or settlement issues.
If there are special travel or resettlement issues the PPs will complete, as appropriate, sections 1, 2, 3, 4 and 5.
The list below (indicative but not exhaustive) highlights some commonly encountered medical conditions which do not warrant the detailed filling in of the resettlement needs section:
- Hypertension, well controlled with medication
- Asthma, well controlled with medication
- Inactive pulmonary tuberculosis
- Syphilis, treated
- Epilepsy under good control
- Diabetes under good control without end organ complications
- Skin conditions/infections (psoriasis, fungal infections)
- Visual acuity deficit of equal or better than 6/15 when corrected
- Radiographic cardiomegaly without clinical manifestations or impairment
In order to preserve medical confidentiality, no personal medical information is to be placed on the resettlement needs section. Thus, the PPs must attempt to get across the basis of the medical problem and the special needs of the refugee without referring to a specific medical diagnosis. This applies as well for psychological assessment of the refugee client which is an important aspect in the evaluation of resettlement needs. This is very important to remember since the information on the resettlement needs section will be made available to people who are not medical professionals.
These 5 sections of the resettlement needs section are:
- Functional Assessment (physical and psychological),
- Special Travel Requirements,
- Post-arrival Service Requirements,
- Housing and Daily Activities or Assistance requirements, and
- Other Resettlement needs.
Section 1: Functional assessment
The functional assessment on the resettlement needs section is clear in identifying major problems that can impact on resettlement of the refugee in Canada (see figure below):

Text version: Section 1: Functional assessment
- Functional assessment: Indicate Yes or No for every listed impairments: Hearing impairment (Partial or Complete); Vision impairment (Partial or Complete); Speech impairment (Partial or Complete); Cognitive impairment (Mild or Moderate or Severe); Mobility impairment (indicate the current mobility aid and the mobility aid required); Other impairment (provide details). Activity of daily living (Independent or Partial care or Total care; provide details).
Note: Please indicate complete when the impairment is complete, and partial when there is a partial impairment. Complete is not meant to indicate that the PP has completed their assessment, it is meant to indicate that the client is completely blind for example, in relation to a visual impairment.
If any of the above noted impairments is present the PPs must indicate “yes”. If they are not present the PPs must check “No”. Even when only one impairment is present, all other answers must be completed with a “No” response.
When there is a positive response to any of these functional assessment questions, the PPs must provide additional information about the impairment (That is, degree of impairment, use of/requirement for a mobility aid). The PPs must also indicate what level of Activities of Daily Living (ADL) the refugee is functioning at and must also add any details that would assist in understanding the degree to which a refugee might be dependent on others for care (for example: the requirement for assistance with feeding, bathing or toileting).
When “Other” functional impairment is marked, remarks are required from the PPs in order to provide information regarding what the problem is, without stating a medical diagnosis.
If the refugee is currently using, or requires, a mobility aid, the nature of that aid must be noted in the space “Current mobility aid” and if the refugee needs a different aid, this must be stated in the option marked: “Mobility aid required”. The most commonly used mobility aids are canes, walkers and wheelchairs.
Finally, if a person is using or would benefit from a mobility aid, the PPs must take this into account when completing section 4, “Housing Requirements” by adding a notation regarding the need for a single level dwelling and/or elevator access.
Section 2: Special travel requirements
The special travel requirements for the refugee to get to their final destination in Canada are listed on the Resettlement needs section (see figure below):

Text version: Section 2: Special travel requirements
- Special Travel Requirements: In the “Special travel requirements” section, select the applicable ones: None, Wheelchair, Stretcher, Medical escort required, Other. Provide details if necessary.
A “Wheelchair” must be indicated whenever the refugee is using or requires a mobility aid. An indication of the size/type of wheelchair required would be helpful. A wheelchair should also be indicated for persons with any medical condition limiting their ability to move quickly or safely when transferring between terminals at an airport. Often this would be the case for persons with mobility problems associated with osteoarthritis, amputation, or cerebral palsy. It should also be considered for persons with cardio-respiratory disorders such as angina, congestive heart failure, valvular heart disease, or chronic obstructive pulmonary disease (COPD).
Please note that request for a “Medical Escort” will be vetted by the Regional Medical Office (RMO) responsible for the refugee’s IME and by IRCC in Ottawa.
If the “Other” option is used, the PPs must provide the specific information in the “Details” section below the responses. Most commonly the option of “Other” will be used when the refugee should be accompanied by an adult family member or might need assistance in undertaking immigration formalities at the Port of Entry in Canada.
It is possible for more than one box to be completed in this section. For example a refugee with severe congestive heart failure might need both a wheelchair during the travel period as well as a medical escort.
Section 3: Post-arrival services required
This section of the resettlement needs Assessment is important as it indicates the actual social and/or medical services that the refugee will require in Canada. Please keep in mind that all refugees will be seen by general practitioners (GPs) in Canada within weeks of their arrival. We are asking PPs to note in this section any requirement for services that would be outside of the services provided by GPs. For example, common diabetes or hypertension are handled by GPs in Canada. Follow up for diabetes would therefore not represent a post-arrival service worth noting.
Social services available in Canada range from special education, speech therapy, occupational therapy, physiotherapy to vocational rehabilitation, attendant care. Social services can also include specialized housing services such as home care and long term care (these housing and care services would require an application to be made and would usually require an assessment by a health professional regarding the need and eligibility for the service). Medical services available in Canada run the full range of specialties and include operative and non-operative care for such medical conditions as cancer, renal failure, coronary artery disease, osteoarthritis, hepatitis and the human immunodeficiency virus (HIV).
In filling in the resettlement needs section, the post-arrival services requirements are either “no services required” or “Consultation with a health care professional required” (see figure below):

Text version: Section 3: Post-arrival services required
- Post-arrival services required. In the “Post-arrival services required” section of the Resettlement Needs section, the requirements are either “no services required” or “Consultation with a health care professional required”. If “Consultation with a health care professional required” is checked, indicate if it is Urgent (72 hrs); Specialized services, Within X weeks, Long term services or As required. Provide details if necessary.
When a consultation is required, the PPs must indicate how quickly that should take place (as shown in the figure above). Again, please keep in mind that post-arrival services worth noting are those provided outside the scope of what GPs would provide.
In deciding on the number of weeks that would be reasonable before the refugee should be seen by a specialist consultant, the PPs must keep in mind that a consultation with a specialist in Canada, can take several weeks and even months to set up. Thus, for a chronic, well controlled, medical condition, one should indicate “as required”.
Long standing conditions that require assessment for a special education class, vocational training, or rehabilitation can also usually be marked “as required”.
Conditions that might benefit from being seen by a specialist in a shorter period of time would be unstable angina or congestive heart failure, or newly diagnosed diabetes needing training of the use of insulin.
In general, almost any refugee requiring a medical escort to accompany them safely to Canada will require an “urgent” specialist assessment. This might include a case of severe COPD requiring oxygen for travel or for everyday use, or a case of severe valvular heart disease requiring stabilisation of secondary heart failure and an “urgent” assessment for consideration of valve replacement surgery. Individuals requiring an assessment for home care or long term residential care must also be marked “urgent”.
If there is any uncertainty with respect to the urgency or time-frame for an Applicant to be assessed by a medical specialist upon arrival to Canada, please contact your Regional Medical Office.
If the refugee’s visual impairment appears to be, or is most likely due to a simple refractive error (most often with younger clients) the best option would be recommendation to see an optometrist. If on the other hand, the visual problem could reasonably be due to cataracts or glaucoma (based on clinical findings or the age of the client) the best option would be referral to an ophthalmologist.
As stated earlier, the “Specialised Services” noted under “Consultation with a health care professional” can refer to needs for such varied social and medical services as:
- special education
- occupational therapy
- physiotherapy
- speech therapy
- vocational training
- lip reading or sign language training
- training for a blind person in navigating his home and community
Long term services can refer to such services as placement of the refugee in a long term care centre for someone who has had a stroke and is not (and will never be) independent in their activities of daily living
Section 4: Housing and daily activities/assistance requirements
The housing and daily activities/assistance requirements section offers the PPs four options for completion (see figure below):

Text version: Section 4: Housing and daily activities/assistance requirements
- Housing and daily activities/assistance requirements. The “housing and daily activities/assistance requirements” section offers the PPs four options for completion: Fully independent, no assistance required; Wheelchair access required; Home care/support services required (Periodically or Permanently); Specialized services required to accommodation functional impairments. Please specify the specialized services required.
The first two options are more or less self-explanatory. The PPs shall keep in mind that someone who does not currently use a wheelchair but who would benefit from one must have the “Wheelchair access required” response checked. This must correspond with a previous positive response regarding “Mobility impairment” in Section 1 of this form.
If the PPs consider that “Home care/support services” are required for a refugee to carry out daily activities in their own home, this must be checked as well as the anticipated frequency of that service. For example, attendant care (for example, nursing care) might be considered necessary for an elderly person who is not able to see well enough to count out daily medications or to give an insulin injection. This would be required daily and permanently. For someone requiring assistance with bathing, the visits by a home care nurse might only be once a week, in which case “periodic” must be checked.
Types of home care services available in Canada are “periodic” and “permanent” (see figure above).
The last option for the PP to consider under Housing and Daily Activities is “Specialized services required to accommodate functional impairments”. This could include long term care in a residential facility with 24-hour nurse staff. Normally this expensive form of residential care is limited to persons who cannot safely function with the more limited nursing services available through home care. Another specialized service might be home oxygen for a refugee with severe COPD.
Section 5: Other comments related to resettlement needs
This section must only be used when relevant details are needed and cannot be written in any of the above sections. Again under no circumstances should a medical diagnosis or information that leads to a medical diagnosis appear on the Resettlement needs section. The PPs must attempt to get across the basis of the medical problem and needs without referring to a specific medical diagnosis.
Once the Resettlement needs section is completed, PPs will submit the completed document electronically. PPs who works on paper IME will date and sign at the bottom of the form indicating their P number and the place where the form was completed.
Example: Section 948 Resettlement needs in eMedical

Text version: Section 948 Resettlement needs in eMedical
In eMedical, Section 948 Resettlement Needs, in the Record results section:
Select the exam date.
- Q1: Does the client have any resettlement/special needs? Select Yes and provide details.
- Q2: Functional assessment
- Q2.1 Hearing impairment (No, Partial or Complete)
- Q2.2 Vision impairment (No, Partial or Complete)
- Q2.3 Speech impairment (No, Partial or Complete)a
- Q2.4 Cognitive impairment (Mild or Moderate or Severe)
- Q2.5 Mobility impairment (indicate the current mobility aid and the mobility aid required)
- Q2.6 Other impairment (provide details).
- Q2.7 Activity of daily living (Independent or Partial care or Total care).
- Q3: Special travel requirements: Select the applicable one: None, Wheelchair, Stretcher, Medical escort required, Other.
- Q4: In the “Post-arrival services required” section, the requirements are either “No services required” or “Consultation with a health care professional required”. If “Consultation with a health care professional required” is checked, indicate if it is: Urgent (72 hrs); Specialized services, Within X weeks, Long term services or As required. Provide details if necessary. Indicate in how many weeks the consultation is required.
- Q5: In the “housing and daily activities/assistance requirements” section offers the PPs four options for completion: Fully independent, no assistance required; Wheelchair access required; Home care/support services required (Periodically or Permanently); Specialized services required to accommodation functional impairments.
- Q6: Do you have any other comment you would like to make in relation to this person’s resettlement needs? Select Yes or No.
Resettlement needs assessment form
B) TIs related to conditions of significance
-
Cancer or malignancy
Subject
Instructions for screening clients with cancer or malignancy in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with cancer or malignancy
- Investigation of clients with cancer or malignancy to help determine their need for medical and/or social services
- Completion and grading of an IME for a client with cancer or malignancy
Instructions
Rationale
Cancer has a major impact on individuals and society. In Canada, health care is delivered through a publicly funded health care system. Cancer care costs are high. Immigration, Refugees and Citizenship Canada (IRCC) is responsible for screening individuals who might reasonably cause excessive demand on health or social services.1 Screening aims to determine the services that will be required by applicants in the foreseeable future.
Screening and testing
Initial screening for all applicants requiring an IME consists of a review of medical history, diagnostic tests, and physical examination. Attention must be paid to signs and symptoms suggestive of malignancy (Appendix A).
Additional investigation
For applicants with a medical history of cancer, PPs must provide the date of diagnosis and last medical follow-up.
If malignancy was previously diagnosed and there has been no treatment and/or recurrence for a period of more than 5 years, a referral to a specialist is not required. If a report from a treating physician is available, include it with the IME. PPs should not request new tests or consultations unless requested by the Regional Medical Office.
Clients who have been diagnosed with cancer or recurrence of cancer within the past 5 years, or underwent cancer-related treatment within the past 5 years, require a medical report from an oncologist. PPs should request and submit any existing specialist reports that include these details:
- diagnosis
- Tumor-Node-Metastasis (TNM) classification and staging
- pertinent investigation reports
- management (including completed, ongoing, and anticipated future treatment needs pertaining to surgery, chemotherapy, radiation therapy, and other medications)
- current clinical status
- prognosis
Clients with a history of treatment for head/neck cancer within the last 5 years (excluding cancer of the Thyroid) have been identified in the latest Canadian Tuberculosis Standards2 as a high risk group for latent tuberculosis (TB) reactivation. These clients require IGRA screening, or TST if IGRA is not available. Consult the TB Technical Instructions and algorithm for further guidance regarding this high risk group.
For clients with IME findings suggestive of malignancy, PPs must note the information on the IME and advise the client to seek appropriate medical care/follow-up as per instructions found in the panel physician handbook.
Reporting
All investigation results and associated reports must be attached to the IME. Any existing specialist reports from previous consultations must also be attached.
In parallel to the IME process, PPs should provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request in accordance with standards outlined by their professional licensing body.
Grading and submission of files
All IMEs for clients with cancer or malignancy must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s), submit the IME with a general comment indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information. Original reports must be translated into English or French before submission.
Algorithm

Cancer and Malignancy TI Algorithm Alternative Text
Screening for cancer and malignancy begins with a medical history, physical examination and diagnostic testing.
Q1: Is there a history OR evidence of cancer/malignancy at the time of the IME?
Yes: If malignancy diagnosed in the past and there has been no treatment and or recurrence for a period of more than 5 years, no referral to a specialist is required. If a report from a treating physician is available, please include it with the IME. PPs should not request new tests or consultations at this time, unless requested by the Regional Medical Office.
For clients who have been diagnosed with cancer or recurrence of cancer within the past 5 years or underwent cancer-related treatment within the past five years, a recent medical report from an oncologist is required.
Clients with a history of treatment for head/neck cancer (except thyroid cancer) within the last 5 years should be screened with IGRA (or TST if IGRA is not available). Consult Tuberculosis Technical Instructions.
Yes to any of the above: Grade B and submit the IME. Attach all additional test results and specialist reports.
References
- Immigration and Refugee Protection Act (A.C. 2001, c27), Part 1, Division 2.0, Sect 16(1)(2)(b)
- Canadian Tuberculosis Standards 7th Edition: 2014
Appendix A
Signs and symptoms of cancer or malignancy
The most common signs and symptoms are fatigue, unexplained weight loss, fever or pain, skin changes, loss of appetite, night sweats, soft tissue or bony masses, enlarged liver on palpation, ascites (abdominal fluid and swelling) and muscle wasting/weight loss.
-
Cognitive impairment in adults
Subject
Instructions for screening clients with possible impaired cognitive functioning in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with possible impaired cognitive functioning (for example, senile dementia)
- Completion and grading of an IME for a client with impaired cognitive functioning
Instructions
Screening and testing
It is important identify clients with cognitive impairment, as well as their specific medical care and social service needs. Such conditions may represent a significant burden and excessive demand on Canadian health services, especially when supportive home care, respite care for family members, and /or placement in a long term care facility is required or anticipated.
During the medical history-taking and physical examination, the PPs must be vigilant for the presence of possible cognitive impairment.
The following information will assist the Regional Medical Office (RMO) in its assessment of the IME:
- Diagnosis/differential diagnosis, and etiology if known
- Duration, stability, and/or progression of symptoms
- Ability to complete activities of daily living and live independently
- Recent medical/health care received (for example, hospitalization, specialist consultations)
- Current and anticipated (over the next 5-10 years) medical care and social service needs (home care, nursing/attendant care, respite care for family members, and/or placement in a long term care facility
- Co-morbidities, such as vascular disease (multi-infarct dementia), electrolyte imbalance, other organic causes of cognitive impairment
- History of neurological problems or associated conditions (e.g. Parkinson’s, Alzheimer etc.)
- Medications: regimen, recent changes
- Drug or alcohol abuse
Additional investigation
An assessment of cognitive functioning and activities of daily living (ADL) is mandatory for all clients aged 75 years and older. For clients with abnormal findings suggestive of cognitive impairment, regardless of age, assessments of ADL and cognitive function must be included.
Reporting
All additional assessment information, including assessments of ADL and cognitive functioning, must be attached to the IME report.
PP’s must not refer clients to specialists unless instructed by the Regional Medical Office. All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME.
Any behaviour suggesting the client may present a danger to self or others must be reported.
In parallel to the Immigration Medical Examination process, PPs are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
All IME’s for clients with abnormal cognitive functioning must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s), submit the IME with a note indicating medical information pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: TI Cognitive impairment in adult
TI Cognitive impairment in adult
IME should be graded B if any abnormalities on medical history and/or physical examination suggestive of cognitive impairment are found.
Q1: Is the client 75 years old or older?
No: Is there any abnormalities on medical history and/or physical examination suggestive of cognitive impairment? If Yes, an ADL and a Screening test for cognitive functioning are mandatory. If No, grade B and submit IME including any existing test results and specialist reports.
Yes: An ADL and a screening test for cognitive functioning are mandatory.
Q2: If the client is = 75 years of age, is there any abnormalities on medical history and/or physical examination suggestive of cognitive impairment?
No: No need for a Screening test for cognitive functioning. Grade B and submit IME including any existing test results and specialist reports.
Yes: An ADL and a Screening test for cognitive functioning are mandatory.
-
Diabetes, hypertension, chronic renal or cardiac diseases
Subject
Instructions for screening of clients with diabetes, hypertension or chronic renal/cardiac diseases in the context of the Canadian immigration medical examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of end-organ damage/renal function impairment in clients with diabetes, hypertension or chronic renal/cardiac diseases
- Investigation of clients with end-organ damage/renal function impairment to help determine their need for medical and /or social services
- Completion and grading of an IME for a client with end-organ damage/renal function impairment
Instructions
Rationale
Long standing diseases such as diabetes, hypertension and chronic renal or cardiac conditions are responsible for end-organ damages and gradual loss of kidney function over time. Chronic renal disease is responsible for a high burden of disease in Canada and lifesaving renal replacement therapies (dialysis and/or kidney transplantation) remain expensive and in short supply.
Screening and testing
During the IME, the PPs must be vigilant in assessing clients with diabetes, hypertension or chronic renal or cardiac diseases for the presence of possible end-organ damage and long term complications, especially renal function impairment. Signs associated with end-organ damage include:
- retinopathy
- neuropathy: check for symptoms or findings such as peripheral neuropathy or pain, autonomic neuropathy (for example, erectile dysfunction, gastrointestinal disturbance, orthostatic hypotension), PPs should include screening via monofilament during foot exam
- Cardiopathy: chest auscultation and radiography is necessary to assess cardiomegaly and cardiopathy
- Nephropathy: special attention should be brought during the IME to blood pressure measure as well as to urinalysis and creatinine results (refer to TIs on urinalysis and serum creatinine)
The identification of clients with end-organ damage and renal function impairment is based on the completion of an appropriate medical history, careful review of risk factors and commonly associated co-morbid conditions, physical examination, and screening investigations.
If an established history of diabetes, hypertension or renal/cardiovascular disease (for example, ischemic heart disease/coronary artery disease, valvular heart disease, cardiomyopathy, cerebrovascular disease [transient ischemic attack, stroke], peripheral artery disease, and /or congenital heart disease) is identified during the IME, the following information will help determine the client’s need for specialized medical care and/or social services.
- Diagnosis
- Duration and progression of symptoms
- New York Heart Association [NYHA] Functional Classification
- Impact on activities of daily living (ADLs)
- Past investigations and treatment /intervention, including hospitalization, surgery, need for renal replacement therapy
- Available specialist reports from past consultations
- Current medications
- Anticipated treatment needed (surgery, dialysis, etc)
Assessment of renal function
Urinalysis is required for all clients ≥ 5 years of age. A urinalysis is also required for clients less than 5 years of age if there is a past history of diabetes, hypertension or kidney disease or if renal function impairment is suspected.
PPs and their clinic staff must NOT directly observe the collection of urine samples. Should there be a concern that a client has provided a falsified sample, the PP should grade the IME B and enter their concerns as a comment.
A serum creatinine level is required for all clients ≥ 15 years of age. A serum creatinine is also required for clients less than 15 years of age if there is a past history of diabetes, hypertension or kidney disease or if renal function impairment is suspected.
Calculation of the estimated glomerular filtration rate (eGFR) is required when serum creatinine is abnormal. (2021 CKD-EPI calculator)
Additional investigation
Clients identified to have impaired renal function (eGFR < 30 mL /min /1.73m2), require the following:
- Urine albumin-to-creatinine ratio (ACR)
Clients with advanced chronic renal failure or end-stage kidney disease (eGFR of <30ml/min at any time during the IME) have been identified in the latest Canadian TB standards as a high risk group for Latent TB reactivation. These clients should therefore be screened with IGRA (or TST if IGRA is not available).
Reporting
PP’s must not refer clients to specialists unless instructed by the Regional Medical Office. All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME.
In parallel to the immigration medical examination process, PPs are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
All IMEs for clients with renal function impairment must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s) submit the IME with a note indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: TI for screening of clients with diabetes, hypertension or chronic renal/cardiac diseases
TI for screening of clients with diabetes, hypertension or chronic renal/cardiac diseases
Q1: Is the client have history or suffer from long standing diseases such as diabetes, hypertension and chronic renal or cardiac conditions?
Yes: An assessment of renal Function is mandatory. A urinalysis and a serum creatinine is required for ALL clients regardless of their age. Continue with Q2.
No: A urinalysis is required for all clients greater (≥) than 5 years of age and a serum creatinine is required for all clients = 15 years of age.
Q2: Is initial urinalysis dipstick shows 1+ for protein or microscopy is normal with protein < 0.30 mg/L and serum creatinine level normal?
Yes: Grade the exam B and submit IME including all additional test results and specialist reports.
No: Repeat urinalysis. If dipstick shows 2+ or 3+ for protein or microscopy is abnormal with protein > 0.30 mg/L. Grade the exam B and submit IME including all additional test results and specialist reports.
Q3: Is serum creatinine level normal?
No: Calculate eGFR. If results are <30 mL/min /1.73 m2, calculate albumin-to-creatinine ratio (ACR) and screened for LTBI with IGRA (or TST if IGRA is not available).
Yes: Grade the exam B and submit IME including all additional test results and specialist reports.
References
-
Debilitating conditions
Subject
Technical Instructions (TI) for screening clients with debilitating conditions in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with a debilitating condition
- Completion and grading of an IME for a client with a debilitating condition
Instructions
Screening and testing
It is important to identify clients with debilitating conditions, as well as their specific medical care and social service needs. Such conditions may represent a significant burden and excessive demand on Canadian health services, especially when supportive home care, respite care for family members, and/or placement in a long term care facility is required or anticipated.
A wide range of chronic diseases may lead to a debilitated state, including the following:
- Neurological diseases: multiple sclerosis, amyotrophic lateral sclerosis (ALS), Parkinson’s, cerebrovascular disease/stroke
- Musculoskeletal and autoimmune diseases: rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), fibromyalgia, other chronic pain conditions /syndromes
- Cardiovascular diseases: peripheral vascular disease +/- amputation, cerebrovascular disease/stroke
- Respiratory diseases: chronic obstructive pulmonary disease, pulmonary fibrosis, oxygen therapy at home
- Some psychiatric conditions: schizophrenia, schizoaffective disorder, bipolar disorder
- Others: advanced cancers; any medical condition with a history of an aggressive course, significant functional impairments, and /or treatment with disease-modifying or biologic therapies
During the medical history-taking and physical examination, the PPs must be vigilant for the presence of debilitating conditions. The identification of clients with debilitating conditions is based on a directed medical history and physical examination. Populations at increased risk include the elderly, patients with long standing chronic diseases (for example, diabetes, hypertension, chronic obstructive pulmonary disease), and/or a family history of cardiac or neurological diseases.
The following information will assist the Regional Medical Office (RMO) in its assessment of the IME:
- Diagnosis/differential diagnosis, and etiology if known
- Duration, stability, and/or progression of symptoms
- Ability to complete activities of daily living and live independently
- Recent medical/health care received (for example, hospitalization, specialist consultations)
- Current and anticipated (over the next 5-10 years) medical care and social service needs (medical treatment, physiotherapy, home care, nursing /attendant care, respite care for family members, and /or placement in a long term care facility
- Medications: regimen, disease modifying and /or biologic therapies
Additional investigation
An assessment of cognitive functioning and activities of daily living (ADL) is mandatory for all clients aged 75 years and older. For clients with abnormal findings suggestive of a debilitating condition, regardless of age, assessments of ADL and cognitive function must be included.
Reporting
All additional assessment information, including assessments of ADL and cognitive functioning, must be attached to the IME report.
PP’s must not refer clients to specialists unless instructed by the Regional Medical Office. All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME.
In parallel to the Immigration Medical Examination process, PPs are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
All IMEs for clients with a debilitating condition must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s), submit the IME with a note indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: TI for Debilitating condition
TI for Debilitating condition
IME should be graded B if any abnormal findings on medical history and /or physical examination suggestive of the presence of a debilitating condition are found.
Q1: Regardless of the age of the client, is there any abnormal findings on medical history and /or physical examination suggestive of the presence of a debilitating condition?
Yes: An ADL and screening test for cognitive functioning is mandatory. Grade B and submit IME including any existing test results and specialist reports.
No: No need to proceed with ADL and screening test for cognitive functioning. Grade B and submit IME including any existing test results and specialist reports.
-
Breast, genital, gynecological and rectal examinations
Subject
Instructions regarding breast, genital, gynecological and rectal examinations of clients as part of the Canadian Immigration Medical Examination (IME).
Instructions
Breast, genital, gynecological and rectal examinations are never indicated in the context of the IME. Panel Physicians are not to conduct these examinations during the IME. If there is a history or a clinical suspicion of breast, genital, gynecological or colorectal malignancy, please make note of it in the medical history portion of the IME.
-
Developmental delay in children
Subject
Instructions for screening children with a possible developmental delay in the context of the Canadian immigration medical examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with possible developmental delay
- Completion and grading of an IME for a child with developmental delay
Instructions
Screening and testing
Developmental delay refers to a significant delay in the process of development and does not refer to a condition where a child is slightly or momentarily lagging in development. The presence of developmental delay is an indication that, without special intervention, the child’s ability to attain normal developmental milestones and educational performance at school is in jeopardy. PPs must be vigilant in their assessment of all paediatric age groups for the presence of possible delays in development, including cognitive, social, speech and language, neurological and behavioural function in children (for example, cerebral palsy, autism, etc.).
The following information should be collected as it will assist medical officers make the determination of current and future (within the next 5-10 years) medical care and social service needs.
- Is there anything in the child’s medical history that would suggest increased risk for developmental delay (that is, complications during pregnancy or delivery, premature delivery, illness, etc.) Please provide details
- Duration, severity, stability, and/or progression of the apparent developmental impairment(s)
- Whether the developmental delay is expected to improve with time, get worse, or stay the same
- Current and future living arrangements (for example, with family or in institutional care facility; who is paying?)
- Need for specialized services (for example, speech and language therapy, occupational therapy, physiotherapy, or supportive home care services) currently or anticipated over the next 5-10 years
- For children = 5 years of age, completion of the Chart of Early Childhood Development (CEDC) is mandatory; please pay particular attention when assessing children known to be at increased risk for developmental issues (that is: premature or difficult birth; illness; trisomy 21, etc.)
- Special education requirements (for example, individualized special education plan, recommended student-to-teacher ratio, or need for an educational assistant)
Additional investigation
When a PP identifies clients with suspected learning disabilities and/or developmental delay, he should provide all relevant information to clarify /confirm the diagnosis, distinguish between medical and social services requirements (for example, medical services at home, special education, occupational therapy, speech language therapy, physiotherapy), and establish a prognosis over the next 5-10 years. This will help the medical officer make the determination of current and future (within the next 5-10 years) medical care and social service requirements of the child.
Reporting
PP’s must not refer clients to specialists unless instructed by the Regional Medical Office (RMO). All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME
In parallel to the immigration medical examination process, PP are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
All IME’s for clients with developmental delay must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s), submit file with a note indicating medical information pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: TI for Developmental Delay in Children
TI for Developmental Delay in Children
IME should be graded B if any abnormalities on medical history and /or physical examination suggestive of developmental delay are found. IME should be submitted including any existing test results and specialist reports.
Q1: Is there any abnormalities on medical history and /or physical examination suggestive of developmental delay?
Yes: Provide all relevant information to clarify /confirm the diagnosis, distinguish between medical and social services requirements (e.g. medical services at home, special education, occupational therapy, speech language therapy, physiotherapy..), and establish a prognosis over the next 5-10 years.
Do not refer client to specialist unless instructed by the RMO.
No: Continue the medical examination.
References
- Look See Checklist by Nipissing District Development Screen (NDDS)
- Ages and Screening Questionnaire (ASQ)
- Parent’s Evaluation of Developmental Status (PEDS) & PEDS: Developmental Milestones
- Learn About PEDSDM/Introduction to PEDSDM
- Canadian Family Developmental Milestones charts
- WHO, Motor development milestones
- CDC, Developmental Milestones chart
-
Hearing impairment or deafness
Subject
Instructions for screening clients who may be deaf or have a significant hearing impairment in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with deafness or hearing impairment
- Investigation of clients with significant hearing impairment to help determine their need for medical and /or social services
- Completion and grading of an IME of a client with deafness or hearing impairment
Instructions
Rationale
The PPs must screen all clients for deafness or hearing impairment and provide additional details of any abnormalities that are identified. This screening is particularly important for children as they may be offered medical /surgical interventions and could require specialized medical and /or social services.
During the medical questionnaire, PPs must be vigilant for the presence of hearing impairment in clients who have the following risk factors:
- Family history of permanent childhood hearing loss (because most hereditary hearing loss is autosomal recessive, many children with hereditary hearing loss may not have affected relatives)
- Admission to a neonatal intensive care unit (NICU) for > 5 days
- NICU stay, regardless of duration, requiring extracorporeal membrane oxygenation, assisted ventilation, exchange transfusion for hyperbilirubinemia, or loop diuretics.
- Congenital or central nervous system infections
- Ototoxic drug exposure, including chemotherapy
- Congenital head and neck deformities (for example, anomalies of the pinna or temporal bone, ear canal, ear tags, ear pits) and /or trauma (particularly basal skull and temporal bone fractures)
- Neurodegenerative disorders
- Genetic syndromes associated with hearing loss (for example, Marfan or Ehlers-Danlos syndromes)
- Chronic or recurrent otitis media with effusion
- Anatomic deformities and other disorders that affect eustachian tube function
During the physical examination, PPs must pay special attention to signs of hearing loss in children, including:
- “Baby talk” is not progressing or speech /language development is delayed or difficult
- Difficulty locating sounds
- Speaks too softly or too loudly
- Turns up the TV volume to an excessively high level
- Behavioural or academic problems; is often classified as being inattentive or disruptive, especially during listening activities
- Often asks, “What?”
- Speech sounds different or child does not speak clearly
- Language is characterized by a reduced vocabulary where words are often missing endings
Several methods can be used in a clinical context to test hearing, depending on a child’s age, development, and health status. Behavioural tests involve careful observation of a child’s behavioural response to sounds such as calibrated speech and tones. The behavioural response might be an infant’s eye movements, a head-turn by a toddler, placement of a game piece by a preschooler, or a hand-raise by a grade-schooler. Speech responses may involve picture identification of a word or repeating words at soft or comfortable levels. Very young children are capable of a number of behavioural tests.
The following questions can be used to identify older children and adolescents for whom a hearing screen may be necessary:
- Do you have a problem hearing over the telephone?
- Do you have trouble following the conversation when two or more people are talking at the same time?
- Do others complain that you turn the television volume too high?
- Do you have to strain to understand conversation?
- Do you have trouble hearing in a noisy background?
- Do you find yourself asking other people to repeat themselves?
- Do many people you talk to seem to mumble (or not speak clearly)?
- Do you misunderstand what others are saying and respond inappropriately?
- Do you have trouble understanding the speech of women and children?
- Do people get annoyed because you misunderstand what they say?
Additional investigation
For children or adults with significant and incapacitating hearing impairment, the PPs must include the following additional information that will assist the Regional Medical Office in its assessment:
- Communication skills used by the hearing impaired client such as lip-reading, signing, reading or writing
- Interpretation of formal audiological testing; and any existing reports from a specialist that details the client’s abilities and specialized service needs (for example, speech and language therapy, hearing aids and /or surgery (cochlear implant)
Reporting
PP’s must not refer clients to specialists unless instructed by the Regional Medical Office. All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME.
In parallel to the Immigration Medical Examination process, PPs are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
All IMEs with significant abnormal findings on the hearing examination must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s), submit the IME with a note indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information.
Algorithm
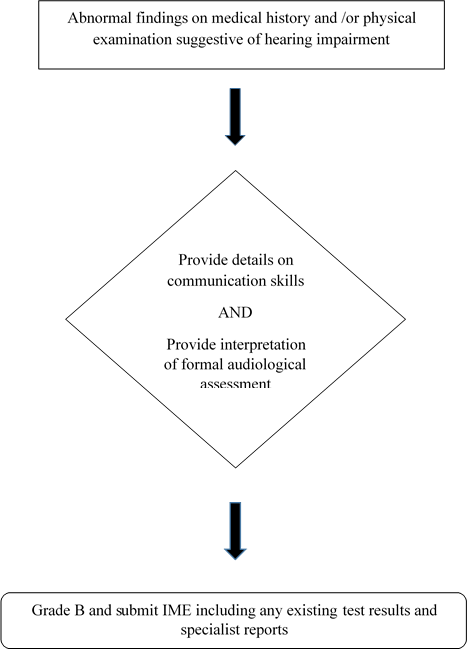
Text version: TI Hearing Impairment or Deafness
TI Hearing Impairment or Deafness
IME should be graded B if abnormal findings on medical history and /or physical examination are suggestive of hearing impairment.
Q1: Is there any abnormal findings on medical history and /or physical examination suggestive of hearing impairment?
Yes: Provide details on communication skills and provide interpretation of formal audiological assessment.
No: Continue with the medical examination.
References
-
Hepatitis/liver disease
Subject
Instructions for screening clients at risk of developing hepatitis/liver disease in the context of the Canadian immigration medical examination (IME).
Goal/objective
These instructions will help to ensure that panel physicians (PPs) follow a consistent and appropriate process for
- identifying clients at risk of developing hepatitis/liver disease
- further investigating clients at risk of developing hepatitis/liver disease
- completing and grading an IME for a client at risk of developing hepatitis/liver disease
Instructions
Rationale
It is particularly important to assess a client’s risk of developing hepatitis/liver disease. These conditions may pose a danger to Canadian public health, and may create a significant burden on Canadian medical services because of the specialized treatment required and the potential need for a liver transplant.
Screening and testing
When taking a client’s medical history and conducting the physical examination, the PP should identify any potential risks of developing hepatitis/liver disease such as hepatitis B or C or liver cirrhosis.
The identification of clients at risk of developing hepatitis/liver disease is based on a careful review of risk factors, medical and surgical histories, and symptoms, as well as a physical examination.
Hepatitis B and C is endemic in many regions of the world from which IRCC clients originate.
- Hepatitis B is endemic in China, South East Asia, the Amazon, eastern and central Europe, sub-Saharan Africa, the Middle East, and the Indian subcontinent.
- Hepatitis C is endemic in Egypt, Pakistan and China.
During the IME, PPs must pay special attention to all clients who have risk factors for hepatitis B and C, particularly those originating from regions where there is a high incidence of hepatitis, as mentioned previously.
Hepatitis B and C testing is required, regardless of age, for clients with any of the following risk factors:
- substance use (includes sharing drug snorting, smoking or injection equipment)
- high-risk sexual activity or a sexual partner with viral hepatitis
- household contact with an infected person, especially if personal items (for example, razors, toothbrushes, nail clippers) are shared
- receipt of unscreened blood products (screening of donated blood products for hepatitis C began in 1990 in Canada)
- needle-stick injury or other occupational exposure (for example, health-care workers)
- children born to mothers with chronic hepatitis B or C infection
- tattoos and body piercing not thought to be done with an aseptic technique
- history of incarceration
- HIV or other sexually transmitted infection
- haemodialysis
Additional investigation is required for some clients as follows:
- All clients with any risk factor for hepatitis B or C must be tested for hepatitis B and C serology (HBsAg and HCV antibodies).
- All clients with a history of hepatitis B or C/liver disease should have their relevant history and treatment(s) noted, as well as any signs of liver decompensation.
- All clients with HIV- or syphilis-positive serotology found during the IME must be tested for hepatitis B and C serology (HBsAg and HCV antibodies).
- For all clients found to have positive serology for hepatitis B or C, results should be recorded, but no further testing is required. Screening for HIV, if not already done, is also required, regardless of age.
Reporting
- Record result of hepatitis B and C testing.
- Record any relevant history related to past and current treatment.
Grading
All IMEs for clients with hepatitis/liver disease must be graded B.
Algorithm
Text version: Hepatitis/liver disease algorithm
PPs must be vigilant for liver disease/hepatitis and should take an appropriate history, review risk factors and conduct a physical examination.
All clients with HIV and/or syphilis or who have a history of, or risk factors for, hepatitis B or C or liver disease, or who have signs and symptoms, should be tested for hepatitis B and C.
If positive: Screen for HIV/syphilis if not already done, regardless of age, and submit IME with reports attached, including relevant history, treatment and signs of liver decompensation.
If negative: Submit IME with reports attached, including relevant history, treatment and signs of liver decompensation.
References
-
HIV
Subject
Instructions for Human Immunodeficiency Virus (HIV) screening in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with HIV infection
- Completion and grading of an IME for a client with positive HIV testing
Instructions
Screening and testing
HIV screening is required for all clients 15 years of age and older undergoing an IME. PPs must also request HIV screening for clients below the age of 15 with any of the following risk factors:
- Signs and/or symptoms compatible with HIV diagnosis
- History of being sexually active
- History of another sexually transmitted infection such as syphilis, herpes, chlamydia, gonorrhea
- History of sharing contaminated needles, syringes and other infected equipment and drug solutions for injection drug use
- History of receiving unsafe injections, blood product transfusions or medical procedures that involve unsterile cutting or piercing
- Accidental needle stick injuries, including among health workers
- Suspected active Tuberculosis, Hepatitis B, Hepatitis C
- Tattoos, body piercing, or acupuncture not thought to be done with aseptic technique
- History of being born to an HIV positive mother; or
- Any child showing failure to thrive
Counselling and consent
Culturally sensitive, age and gender appropriate pre- and post-test counselling should be provided with consideration given to relevant legal, ethical, social and human rights issues. If an interpreter is used, PPs must select and ensure that the interpreter is unbiased and has no connection to the client. Family members or friends cannot act as interpreters for clients. The use of a professional interpreter is at the client’s expense.
Detailed information on pre- and post-test counselling parameters can be found in the International Organization for Migration (IOM) Guide for HIV Counsellors: IOM HIV Counselling in the Context of Migration Health Assessment.
PPs should provide pre-test counselling (see the example in Annex 1 below; Ontario Public Health form for an example of an HIV requisition ) that includes information on the following:
- Means of HIV transmission and prevention
- Description of testing procedure
- Confidentiality of HIV testing, reporting, and record handling
- Meaning of HIV screening test results, including the possibility of false positive or false negative results
- Need to inform anyone at risk of infection if the test is positive
- Client’s consent to undergo testing
For all clients with positive HIV testing, PPs must provide a completed (signed and dated) Acknowledgement of Post-test Counselling form (Annex 2). Only the post-test counselling form must be documented on the IME.
Testing
Only laboratories trained and equipped for HIV testing, including those using validated laboratory tests recommended by Health Canada or the World Health Organization (WHO) should be used.
Further details on rapid HIV serological tests are available.
Results and reporting
An indeterminate or reactive (that is, positive) test result should be repeated automatically by the laboratory using a different assay on the same blood specimen prior to reporting the initial result.
For results that are discordant (that is, first test is reactive, and the second assay is non-reactive) the same blood specimen should be tested by means of a third assay (different from the first and second assays using the same specimen). A positive result at this point would confirm HIV seropositivity.
If the final test result on the first blood specimen remains indeterminate, then a repeat HIV test (second blood specimen) is mandatory. If the final test result of the repeat specimen is indeterminate (that is, two indeterminate final results), the reports should be submitted with the IME.
The post-test counselling form must be completed by the PP. IME results must be forwarded directly to IRCC with all laboratory test results attached.
Post-Test Counselling for Negative Results
A single negative result does not preclude the possibility of HIV infection, but is acceptable as an initial test for IME purposes. Post-test counselling after a negative HIV test result is recommended, but not mandatory for IRCC purposes. This would include providing information on the importance of risk reduction. PPs should indicate whether they believe that there may be a high risk of a false-negative result.
Post-Test Counselling for Positive Results
An applicant with a confirmed positive HIV result requires the following information collected:
- CD4 count
- HIV viral load
- hepatitis B screening (HBsAg)
- hepatitis C screening (HCV Ab)
- a completed (signed and dated) Acknowledgement of HIV Post Test Counselling form (in Annex 2) even if the applicant is already aware that they are HIV (+)
- antiretroviral medication regimen including drug name(s), dose(s) and frequency of administration
*if this is a new diagnosis of HIV and / or the applicant is not currently on an antiretroviral regimen, the RMO may further for an HIV Expert report (HIV specialist or a physician with a special interest and knowledge of HIV treatment)
IGRA testing
According to The Canadian Tuberculosis Standards 8th Edition Chapter 10, all patients with newly diagnosed HIV infection should be assessed for the presence of active TB. HIV positive individuals are also at high risk of reactivation of latent TB and thus should be screened for LTBI (Please refer to the Technical Instructions “Tuberculosis” for guidance on active TB and LTBI screening). TB risk is increased regardless of CD4 count in HIV-infected persons and typical clinical or radiologic features may be absent. Hepatitis B and C screening must also be done for all HIV-infected persons as they are important conditions of co-morbidity.
Grading and submission of files
All IMEs for clients with abnormal HIV serology must be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s), submit the IME with a note indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: TI for HIV
TI for HIV
Q1: Is the client 15 years or older?
Yes: Performed an initial screening for HIV with an ELISA test
No: Performed an initial screening for HIV only if client present signs and /or symptoms of or risk factors for HIV (refer to list under ‘Screening and Testing’).
Q2: Is the initial HIV results negatives
Yes: Submit IME and all laboratory reports
No: Continue with Q3 if results are positives or Q4 if results are indeterminate.
Q3: Is the initial HIV results are confirmed positive?
Yes:
- Screen for Hepatitis B and C, Syphilis and CXR (PA for adult and AP + lateral if < 11yo) if not already done.
- Screen for LTBI: request IGRA or TST if IGRA not available
- Grade B and include signed Post-test counselling form
No: If results are negatives, submit IME or continue with Q4 if results are indeterminate
Q4: Is the initial HIV results are indeterminate?
Yes: Repeat test on a new blood specimen required by ELISA or Western Blot
No: Refer to Q2 or Q3
Q5: Is the results of the repeated HIV tests confirmed positive?
Yes:
- Screen for Hepatitis B and C, Syphilis and CXR (PA for adult and AP + lateral if < 11yo) if not already done.
- Screen for LTBI: request IGRA or TST if IGRA not available
- Grade B and include signed Post-test counselling form
No: Submit IME and all laboratory reports
References
- HIV and AIDS (who.int)
- Canadian Guidelines on Sexually Transmitted Infections, Section 5-8: Human Immunodeficiency Virus Infections. Public Health Agency of Canada (PHAC), 2016.
- Canadian Provincial/Territorial STI Guidelines
- WHO Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach
- IOM Guide for HIV Counsellors: IOM HIV Counselling in the Context of Migration Health Assessment | IOM Publications Platform
- A guide to monitoring and evaluation for collaborative TB/HIV activities (who.int)
- Global HIV/AIDS Overview
- HIV Treatment | CATIE - Canada's source for HIV and hepatitis C information
- Prevention of mother-to-child transmission (PMTCT) of HIV
Annex 1: Pre-test counselling
Pre-test counselling (PDF, 731.31 KB)
Click on HIV Serology Requisition Form (PDF, 731 KB) - new (as of Feb 5, 2018)
Annex 2: Post-test counselling form
Acknowledgement of HIV post-test counselling (IMM 5728) (PDF, 1.54 MB)
-
Psychiatric conditions
Subject
Instructions for screening immigration clients with psychiatric conditions in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with psychiatric illness
- Assessment of clients with a suspected or confirmed specific psychiatric conditions such as depressive disorder, psychotic disorder, substance use disorder, and /or antisocial behaviour in order to determine their risk to public safety and their potential need for medical and /or social services
- Completion and grading of an IME for a client with a psychiatric condition
Instructions
Screening and testing
During the IME, PPs must assess all clients for mental health. The identification of psychiatric illness is important in order to provide the information required for the medical officer to assess the client’s potential risk to Canadian public safety, and demand on Canadian medical /social services.
Diagnostic criteria for individual psychiatric conditions can be found in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
- Anxiety disorders, personality troubles or mild mood disorders requiring no or minimal follow up and that have no impact on public safety are quite common. These conditions do not represent a demand on Canadian medical/social services and as such, should be noted by the PP on the IME in the 501-Medical Examination: Detailed Questions; Mental and Cognitive state. No additional investigation is required
- Depression is the most common psychiatric disorder in the general population. Again, the PP should assess the depressive disorder in terms of risk to public safety and the level of services required by the client. A variety of screening instruments are available, but their reliability can be affected by the client’s interpretation of mental health terms and their cultural conception of symptomatology. An awareness of the terms used by a particular population to describe emotional issues, as well as the relevancy of particular questions in determining an individual’s mental state, could facilitate the identification of depression in such groups. Despite some of their limitations, depression screening tools remain valuable in the identification of immigration applicants possibly suffering from a depressive disorder. A commonly used short screening tool for depression is the PHQ-9 (Patient Health Questionnaire)
- Psychosis, broadly defined as the loss of contact with reality, can be accompanied by delusions and /or hallucinations and is associated with an increased risk of the individual harming themselves or others. PPs must provide information concerning whether the applicant is likely to mount a harmful action in response to a psychotic disturbance
- Substance use disorders are important to identify due to their association with antisocial and criminal behaviours, as well as their ability to induce mood disturbances and psychosis. Substances of abuse include, but are not limited to: alcohol, marijuana, opioids, cocaine, methamphetamine, benzodiazepines, caffeine, tobacco, and prescription /over-the-counter medications. If a substance use disorder is identified, it is important to document the route of use, frequency of use, amount per use, last use, and whether any rehabilitation treatment has already been required and/or is anticipated. Include any past history and potential further risk for impaired driving
Screen for conditions of public safety concern
A condition of public safety concern refers to a mental health condition in an individual, for which the examining physician is of the opinion that the person is likely to cause harm to others. Screening for psychiatric conditions of public safety concern in a diverse population is challenging. It is important to identify clients with mental health disorders to determine whether they are likely to pose a danger to Canadian public safety.
To further aid PPs, a current or past history of any of the following characteristics might suggest that the individual could pose a danger to Canadian public safety:
- Delusional behaviour, or a diagnosis of schizophrenia or schizoaffective disorder
- Antisocial, violent, or impulsive behaviour (including impaired driving)
- Paranoid ideas or odd beliefs
- Homicidal or suicidal thoughts
- Substance use disorder
- Memory disturbance
- Psychological or physical trauma, including post-traumatic stress disorder (PTSD)
- Aberrant sexual disorders, such as pedophilia
Screen for demand on social and/or medical services
PPs must screen clients for conditions that might result in an increased need for social and /or medical services (excessive demand). Psychiatric conditions, sometimes regardless of treatment, can significantly impair an individual’s social, academic, and /or occupational functioning. In such cases, the individual might require extended medical rehabilitation and access to a variety of supportive social services. Therefore, it is important for PPs to provide information that could help clarify the applicant’s ability to live independently and maintain employment. In cases of established psychiatric illness, PPs must comment on whether the applicant has been assessed by a psychiatrist, whether they are followed by a treating physician (for example, psychiatrist or family doctor), whether hospitalization has been required for the condition (if so, when and how often?), and whether the condition is likely to remain stable, improve, or worsen. It should also include a description of investigations, treatments and services that will likely be required in the future (for example, medication, hospitalization, detoxification treatment, long term care facility admission, special programs etc.)
Reporting
PP’s must not refer clients to specialists unless instructed by the Regional Medical Office. All existing lab results and/or any specialist reports from previous specialist consultations must be attached to the IME.
Medication prescribed for psychiatric conditions (for example, SSRIs and other antipsychotics should all be noted in the 501 Medical Examination: Medical History.
Anxiety disorders, personality troubles or mild mood disorders requiring no or minimal follow up and that have no impact on public safety should be noted on the IME in the 501-Medical Examination: Detailed Questions; Mental and cognitive state. No additional investigation is required.
In cases where a mental health condition is identified and possible risk to public safety and /or increased need for social/medical services is suspected, the PP should provide all available reports (psychiatry, psychology /psychotherapy, treating family doctor, social worker, etc.). PP should also note in the IME his own assessment of the condition; this should include history of the mental condition, a full description of current symptoms, expected investigations and treatment (including medication, hospital admissions, out-patient visits etc.) as well as an evaluation of any behaviour that could potentially be harmful to self or others.
PP should indicate if an evaluation in psychiatry is suggested to further evaluate the client. PP’s must not refer clients to specialists unless instructed by the Regional Medical Office.
In parallel to the Immigration Medical Examination process, PPs are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
All IMEs for clients with evidence of mental health disorders must be graded B.
All files are to be submitted within the 10-day client service standard. In cases where report(s) are pending, submit the IME with a note indicating that additional medical information is pending. The Regional Medical Office will create a ‘furtherance request’ for the pending information.
Algorithm

Text version: TI for Psychiatric Conditions
TI for Psychiatric Conditions
IME should be graded B if abnormal findings on medical history and /or physical examination suggests a mental health condition associated with potential risk to Canadian public safety or potential increased need for social/medical services.
Q1: Is there abnormal findings on medical history and /or physical examination suggests a mental health condition associated with potential risk to Canadian public safety or potential increased need for social/medical services?
Yes: Provide full assessment and include history of the mental condition, a full description of current symptoms, expected investigations and treatment (including medication, hospital admissions, out-patient visits etc) as well as an evaluation of any behaviour that could potentially be harmful to self or others.
Provide any available reports (psychiatry, psychology /psychotherapy, treating family doctor, social worker, etc.).
Indicate if an evaluation in psychiatry is suggested to further evaluate the client. PP’s must not refer clients to specialists unless instructed by the Regional Medical Office.
Grade B and submit IME including any additional test results and specialist reports
No: Complete the IME following the normal process.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, 5th edition (DSM-5). Arlington, VA: American Psychiatric Publishing.
- British Columbia Ministry of Health and CARMHA. (2008). Family Physician Guide: For Depression, Anxiety Disorders, Early Psychosis and Substance Use Disorders. (PDF, 9.31 MB)
- British Columbia Ministry of Health. (1999). Patient Heath Questionnaire (PHQ-9) (PDF, 41.03 KB)
-
Syphilis
Subject
Instructions for syphilis screening in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with syphilis infection
- Further investigation of clients with positive syphilis testing to ensure that appropriate treatment has been completed prior to entry into Canada
- Completion and grading of an IME for a client with positive syphilis testing
Instructions
Screening
Syphilis screening is required for all clients 15 years of age and older undergoing an IME. PPs must also request syphilis testing for clients below the age of 15 with any of the following risk factors:
- Signs and /or symptoms compatible with syphilis infection (see table below)
- High risk sexually activity (for example, unprotected anal or vaginal sex, multiple sexual partners)
- History of another sexually transmitted infection such as HIV, herpes, chlamydia, gonorrhoea
- History of being born to a mother diagnosed with syphilis
- History of sexual contact with a known case of syphilis
- History of pregnancy
- Men having sex with men
- Sex workers
- Injection drug users
The evaluation consists of a medical history, physical examination and laboratory tests. Panel physicians are required to report signs and symptoms related to syphilis, previous syphilis diagnosis and evidence of recent or previous treatment. Symptoms are non-specific and it is entirely possible to go through the early stages of the infection without knowing about it.
Syphilis, signs & symptoms Stages Signs and symptoms Primary Chancre, usually at the site of inoculation (for example, genitals, anus, mouth) after a mean incubation period of 21 days. Secondary Mucocutaneous lesions, rash affecting palms and soles, condylomata lata, non-specific constitutional symptoms such as malaise, fever and lymphadenopathy. Latent Asymptomatic, positive syphilis serology with no clinical signs and symptoms. Tertiary: Neurosyphilis, Cardiovascular syphilis and Gummatous lesions (gumma) Acute changes in mental status, meningitis, stroke, cranial nerve dysfunction and auditory or ophthalmic and ocular abnormalities. Late neurosyphilis occurs 10–30 years or more after infection characterized by tabes dorsalis and general paresis
Aortic aneurysm, aortic regurgitation, coronary artery ostial stenosis
Tissue destruction of any organ; manifestations depend on the affected site
Congenital Syphilis Signs of early congenital syphilis include bullous rash, rhinitis, laryngitis, lymphadenopathy, hepatosplenomegaly, osteochrondritis, periostitis, meningitis and chorioretinitis
The signs of late congenital syphilis infection in children over the age of 2 years include inflammatory manifestations affecting the eyes, ears and joints, as well as skeletal malformations and stigmata resulting from developmental damage during the early stages of syphilis.
Testing
Several tests are available to screen for Treponema pallidum, the bacteria that causes syphilis. There are 2 categories of serologic tests to detect syphilis: Non-treponemal tests and Treponemal-specific tests.
Non-treponemal tests detect antibodies often associated with, but not specific to, syphilis infection. These tests provide semi-quantitative results, which can be used to assess response to treatment. Non-treponemal tests include: rapid plasma reagin (RPR); venereal disease research laboratory (VDRL), and toluidine red unheated serum test (TRUST).
Treponemal tests detect antibodies specific to T. pallidum. These antibodies can remain after treatment. Treponemal tests include: T. pallidum enzyme immunoassay (EIA), T. pallidum chemiluminescence immunoassay (CIA), T. pallidum particle agglutination assay (TPPA), fluorescent treponemal antibody absorption (FTA-ABS), and microhemagglutination test for antibodies for T. pallidum (MHA-TP). Unlike most Non-treponemal tests, Treponemal tests are often automated and are now frequently being used in the initial screening tests for syphilis.
Results
Historically, a Non-treponemal or a Treponemal test could be used for initial syphilis screening and the type of test used is dictated by the clinical laboratory. A majority of the Canadian provincial public health laboratories now utilize one of the following Treponemal assays as an initial syphilis antibody screening test: EIA or CIA. If this initial antibody screen is non-reactive (negative), then no further testing is required. If the antibody screen is reactive (positive), confirmatory testing with both the RPR and TPPA must be performed on the same blood sample. This is the preferred syphilis testing algorithm. The RPR is particularly helpful in differentiating acute from latent or remote syphilis infection and can be used to identify reinfection and monitor response to treatment. Interpretation of serology results can be complex. Consult with your local laboratory regarding testing protocols and interpretation of results.
If neither of the EIA or CIA syphilis antibody tests are available in the PP’s jurisdiction of practice, the PP can opt to request non-Treponemal tests as the initial syphilis screening test. If the initial screening is reactive, confirmatory testing on the same blood sample with TPPA (or FTA-ABS) must be performed. If the initial screening is non-reactive, then no further testing is required unless there is clinical suspicion of early syphilis. If clinical suspicion of early syphilis is present, repeat syphilis testing RPR (or VDRL) with TPPA (or FTA-ABS) on a new blood sample 4 weeks after initial screening test.
Indeterminate or discordant results (initial test reactive and second test non-reactive) are to be repeated on a new blood sample 4 weeks after the initial screening test. In these situations, the IME should be submitted within 10 days of the initial exam with a note indicating further results will be provided once available.
Treatment
Syphilis is completely curable with antibiotics. If untreated, it is a public health risk mainly due to sexual transmission during the early stages of infection or through transmission of infection from mother to fetus (congenital syphilis). In some untreated individuals, long term serious complications can occur.
For the purpose of the IME, all cases of syphilis infection must be adequately treated and proof of this treatment is required (Form IMM 5965 E — Appendix A). PPs should provide treatment that is consistent with accepted syphilis treatment guidelines (World Health Organization, Canadian Guidelines on Sexually Transmitted Infections)Footnote 1. If the PP is not able to provide treatment, they should refer the client to a healthcare provider who can provide treatment.
The appropriate treatment regimen will depend on the client’s stage of syphilis infection. Per the Canadian Sexually Transmitted Infections Guidelines:
- Infectious syphilis (primary, secondary and early latent stages): Long-acting Benzathine Penicillin G 2.4 million units intramuscular (IM) as a single dose.
- Longer duration syphilis (late latent and tertiary syphilis): Three (3) weekly doses of Benzathine penicillin G-LA 2.4 million units IM.
- Neurosyphilis requires more aggressive treatment with intravenous antibiotics, and should be managed by, or in consultation with, an infectious disease specialist.
In asymptomatic seropositive individuals who lack a clear history of prior syphilis infection or treatment, the diagnosis is late latent syphilis or latent syphilis of unknown duration. The treatment for late latent syphilis and latent syphilis of unknown duration is the same and acceptable regimens are:
- Benzathine penicillin G 2.4 million units IM weekly for 3 consecutive weeks; or
- Doxycycline 100 mg PO bid for 28 days; or
- Ceftriaxone 1 g IV or IM daily for 10 days (only in exceptional circumstances)
If a client testing positive for syphilis indicates a previous history of syphilis treatment, the client should be referred to the local public health authority to determine if the testing result is compatible with a new infection (reinfection) and if a new course of treatment is required. IRCC requires: regimen, dosage, and dates of administration.
Proof of treatment information should be noted in the General Supporting comments of the 712 - Syphilis test section or a report may be attached to the IME.
Public health reporting
Syphilis is a reportable disease in Canada and elsewhere. Follow the direction of your local public health authority in order to meet public health reporting requirements.
Reporting of results to IRCC
All additional lab result reports must be attached to the IM. Any specialist reports from previous consultations must also be attached.
For cases with negative screening: submit and include copy of test results if performed in laboratory.
For cases with positive screening: submit with copy of tests results and proof of treatment (also add a note in the General Supporting comments of the 712 - Syphilis test section).
For cases with indeterminate or discordant results (initial test reactive and second test non-reactive), submit the file indicating “Indeterminate (or discordant) results, Syphilis testing will be repeated in 4 weeks. Please create Furtherance”.
If not already done, Hepatitis B and C testing is required for all clients who screened positive for syphilis.
In parallel to the Immigration Medical Examination process, PPs are to provide appropriate and timely advice to the client when they discover a serious medical condition not known to the client. In doing so, they are to uphold professional and ethical standards by referring the client back to their usual treating physician or to an appropriate specialist upon request.
Grading and submission of files
All IMEs for clients with abnormal syphilis serology should be graded B.
All files are to be submitted within the 10 day client service standard. For cases with pending report(s), submit the IME with a note indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: TI for Syphilis
TI for Syphilis
All IMEs for clients with abnormal syphilis serology should be graded B.
Preferred Testing Algorithm
Q1: What is the result of the treponemal test Antibody screening with either EIA or CIA?
If non-reactive: Submit the IME including all available test results and specialist reports
If reactive: Proceed to a confirmatory testing on the same blood sample with RPR and TPPA.
Q2: What is the result of the confirmatory testing on the same blood sample with RPR and TPPA?
If indeterminate /Discordant Results: Repeat syphilis testing: EIA or CIA with RPR and TPPA on a new blood sample 4 weeks after the initial screening test. Continue with Q3.
If reactive: Provide a proof of appropriate syphilis treatment, serology for HIV, Hepatitis B and C serology (if not already completed). Submit the IME including all available test results and specialist reports.
Q3: What is the result of the repeated syphilis testing 4 weeks after the initial screening test?
If reactive: Provide a proof of appropriate syphilis treatment, serology for HIV, Hepatitis B and C serology (if not already completed). Submit the IME including all available test results and specialist reports.
If indeterminate /Discordant Results: Submit the IME including all available test results and specialist reports.
Alternative Testing Algorithm
Q1: What is the result of the Non-Treponemal test: RPR (or VDLR)?
If non-reactive: Do you have clinical suspicion of early syphilis infection? If No, submit the IME including all available test results and specialist reports. If Yes, repeat syphilis testing: RPR (or VDRL) with TPPA (or FTA-ABS) on a new blood sample 4 weeks after initial screening test and continue with Q3.
If reactive: Proceed with a confirmatory testing on the same blood sample with TPPA (or FTA-ABS)
Q2: What is the result of the confirmatory testing on the same blood sample with TPPA (or FTA-ABS)?
If indeterminate /Discordant Results: Repeat syphilis testing: RPR (or VDRL) with TPPA (or FTA-ABS) on a new blood sample 4 weeks after initial screening test. Continue with Q3.
If reactive: If confirmed reactive, provide proof of appropriate syphilis treatment, serology for HIV, Hepatitis B and C serology (if not already completed). Submit the IME including all available test results and specialist reports.
Q3: What is the result of the repeated syphilis testing 4 weeks after initial screening test?
If reactive: Provide proof of appropriate syphilis treatment, serology for HIV, Hepatitis B and C serology (if not already completed). Submit the IME including all available test results and specialist reports.
If indeterminate /Discordant Results: Submit the IME including all available test results and specialist reports.
References
-
Tuberculosis
Subject
Instructions for screening clients to detect active or latent pulmonary tuberculosis infection (LTBI) in the context of the Canadian Immigration Medical Examination (IME).
Goal/objective
This document provides guidelines, instructions and algorithms for the screening and diagnosis of active and LTBI according to the latest Canadian Tuberculosis Standards2 and World Health Organisation (WHO) guidelines on TB.3
These instructions are provided to ensure that panel physicians (PPs) follow a consistent and appropriate process for the following:
- Identification of clients with active TB or LTBI
- Investigation of clients where there is clinical suspicion of active TB or LTBI
- Investigation of clients who are close contacts of an individual with active TB
- Identification and investigation of high risk clients for TB
- Referral to a specialist for further investigation and treatment of suspected active or latent TB
- Completion and grading of an IME of a client with active TB or latent LTBI
Instructions
Particular attention must be paid to signs, symptoms and risk factors suggestive of active tuberculosis. Some of the strongest predictors of active TB include the country of origin, living conditions, recent contact with active TB and medical comorbidities (Appendix A)4. The following instructions apply to all clients who require an IME.
- Screen all clients for tuberculosis during the review of medical history and physical examination.
- Require a postero-anterior chest x-ray (CXR) for all clients ≥ 11 years of age.
- Require an antero-posterior and lateral CXR for all clients < 11 years of age with a previous history of TB infection/treatment who are in a high risk group for TB as defined below.
- Perform the tuberculosis screening algorithm to detect TB.
- Require Interferon Gamma Release Assay (IGRA) testing (or Tuberculin Skin Test [TST] if IGRA is not available) for clients who are in the following 5 TB High Risk Groups:
- Clients who have been in close contact with an active TB case within the previous 5 years (Appendix A)
- Clients with HIV positive serology
- Clients with a history of head and neck cancer within the last 5 years (i.e. cancer of the oral cavity, salivary glands, larynx, pharynx, nasal cavity or paranasal sinuses). Note: thyroid cancers are not considered high risk
- Clients with advanced chronic renal failure or end-stage kidney disease (eGFR of <30 mL /min /1.73m2 at any time during the IME)
- Clients with a solid organ or bone marrow transplant on immunosuppressant therapy. Note: immunosuppressant therapy outside of solid organ and bone marrow transplant is not included in this risk group at the moment.
Tests required for clients who are in the above 5 High Risk Groups
1. 950 – IGRA/TST testing
For clients = 2 years of age, IGRA testing is required using one of the following two tests: QIAGEN QuantiFERON® for TB (or any iteration, such as QuantiFERON-TB Gold Plus) or OXFORD IMMUNOTEC T-SPOT®.TB. For immigration purposes, an indeterminate, borderline, or weakly positive IGRA results should be reported as negative.
The tuberculin skin test (TST) can be used in place of IGRA only if both of the above mentioned 2 IGRA products are not licensed in the country of practice.
For clients < 2 years of age, a TST should be performed using purified protein derivative (PPD) administered intradermally by the Mantoux method. Preparations used should be equivalent to 5TU.
A TST positive result is a measured induration = 5mm read 48 to 72 hours after planting the PPD. Clients with documented positive PPD results should be reported as positive and PPs should proceed with the algorithm.
For clients that do not have any of the high risk conditions, an induration = 10 mm is clinically used for positive results.
2. 502 - CXR
A PA CXR will have already been completed for clients ≥ 11 years of age.
For clients < 11 years old, complete a 502-AP CXR and a 510-Lateral. AP CXR exams do not currently exist in eMedical so PPs will need to specifically request an antero-posterior view from the radiologist rather than a postero-anterior view.
Clients who test positive for LTBI screening and/or have CXR lesions = 4.1 and/or have symptoms of active TB must undergo steps 3 and 4.
3. 601 - Sputum smears & cultures (x3)
If available, molecular testing for Mycobacterium tuberculosis (MTB) based on nucleic acid amplification (NAAT) must be performed on the first specimen when all acid-fast bacilli (AFB) smears are negative OR on one of any specimen with a positive smear (Appendix B).
4. 707 – HIV
HIV screening will have already been completed for all clients ≥ 15 years of age.
Clients < 15 years of age with active TB or clients who are part of the high risk group and who have a positive IGRA/TST result must also be screened for HIV.
HIV and TB are often comorbid conditions and their screenings should be done hand in hand. All patients with HIV infection are at high risk of reactivation of latent TB and should be assessed for the presence of active TB. TB risk is increased regardless of CD4 count in HIV-infected persons and typical clinical or radiologic features may be absent.
Following the same logic, all clients testing positive for active TB or LTBI should be screened for HIV regardless of age.
5. 602 TB specialist report
Clients with positive sputum results should be referred to a TB specialist for further investigations.
A TB specialist is defined as a physician with experience or expertise sufficient to evaluate, diagnose and treat tuberculosis. The TB specialist report should contain the following information:
- a report clarifying /confirming the applicant’s diagnosis and management /treatment needs
- results of sputum testing (three sputum samples [induced, if necessary]) for AFB smear microscopy and Mycobacterial culture)
- follow-up PA chest x-ray image
- if active pulmonary TB is confirmed, provide treatment details (drug regimen, start date, and expected duration)
- all follow-up investigations (repeat sputum testing to confirm conversion to negative, repeat PA chest x-ray images)
If the client is already managed by a specialist at the time of the TB investigation or has a previous report available, do not re-refer clients unless clinically indicated. Submit all pertinent reports with the IME. If a previous report is not adequate or sufficiently current, the case will be furthered at the discretion of the Regional Medical Office (RMO) for additional follow-up with a TB specialist.
Applicants diagnosed with Active Tuberculosis must be treated according to recognized guidelines such as the Canadian Tuberculosis Standards2, the Communicable Disease Network Australia (CDNA) 8, UK NICE 9, the USA Centers for Disease Control and Prevention (CDC) 10 or the World Health Organization (WHO).11, 12 Although Directly Observed Therapy is not mandatory, applicants should be informed that it is highly recommended.
6. Contact Tracing
If a person infected with pulmonary tuberculosis is identified during the course of the IME, it is imperative to conduct contact tracing on the family members of the index case. Any client that meets the definition of a close contact (Appendix A) and requires an IME is considered part of the high risk group and must undergo screening as outlined in the instructions.
PPs should notify the RMO as soon as possible if IMEs have already been completed and submitted for family members who require contact tracing.
Results and reporting
All IMEs for clients with active, latent or symptoms of pulmonary TB must be graded B. All results and specialist reports must be attached to the file. General comments should be entered as per the algorithm.
When indicated, tuberculosis screening with sputum testing should be requested. If it is not possible to obtain sputum samples or if procedures require a specialist referral, submit file with a note indicating: “Applicant unable to produce sputum” or “Specialist referral required”. The RMO will provide further instructions.
Any previous chest x-rays or specialist reports available should be submitted with IME.
For results and reporting for contact tracing, go directly to the contact tracing algorithm below.
Grading and submission of files
All IMEs for clients with active, latent or symptoms of pulmonary TB must be graded B. All results and specialist reports must be attached to the file. General comments should be entered as per the algorithm.
All files are to be submitted within the 10-day client service standard. For cases with pending report(s), submit the IME with a note indicating additional medical information is pending. The RMO will create a furtherance request for the outstanding information.
Algorithm

Text version: Pulmonary Tuberculosis Screening Algorithm
All clients are screened for TB during medical history taking, physical examination and CXR (= 11 years)
Active TB
Q1: Is there suspicion of Active TB and /or CXR graded = 4.1?
Yes: Order 601 Sputum AFB smears and Mycobacterial cultures X 3. Nucleic acid amplification testing for Mycobacterium tuberculosis (MTB NAAT) should be performed on the first specimen when all AFB smears are negative OR on any specimen with a positive smear.
No: Grade and Submit the IME.
Q2: Is the sputum smear or MTB NAAT result positive?
Yes: Attach results. Add a general comment: "Active TB screening, smears positive, cultures pending". Order 707-HIV test if not already done. Refer to TB specialist. Initiate contact tracing. Grade B and submit IME.
No: Attach results. Add general comment: "Active TB screening, smears negative, cultures pending". Grade B and submit IME.
Client with TB High Risk Condition*
Q1: Does the client have any of the 5 high risk conditions?
Yes: Order 950 – IGRA if = 2 years of age or TST if the client is < 2 years AND clients < 11 years of age require a 502-AP CXR and 510-Lateral CXR
No: Proceed with standard IME screening
Q2: Are ALL the results negative (IGRA, TST <5mm, CXR < 4.1 and no suspicion of TB)?
Yes: Attach results. Add general comment: "High risk group, LTBI screen negative, sputum smears/cultures not indicated". Grade B and submit IME.
Q3: Are ANY of the results positive (IGRA, TST > 5mm, CXR =; 4.1 or a suspicion of TB)?
Yes: Order 601 Sputum AFB smears and Mycobacterial cultures X 3. MTB NAAT should be performed on the first specimen when all AFB smears are negative OR on any specimen with a positive smear AND 707 – HIV test, if not already done.
Q4: Are the sputum smears and/or MTB NAAT positive?
Yes: Attach results and reports. Add General Comment:" High risk group, LTBI screen positive, sputum smear positive (or negative), cultures pending". Refer to TB specialist. Initiate contact tracing. Grade B and submit IME.
No: Attach results and reports. Add general comments: "High risk group, LTBI screen positive, sputum smears negative, cultures pending". Grade B and submit IME.
Text version: Contact Tracing Algorithm
Clients require 950 – IGRA if = 2 years of age or TST if the client is < 2 years AND clients < 11 years of age require a 502-AP CXR and 510-Lateral CXR.
Q1: Are ALL the results negative (IGRA, TST <5mm, CXR < 4.1)
Yes: Attach results. Add general comment: "Contact tracing completed, results negative". Grade B and submit IME.
No: If any of the results are positive (IGRA, TST > 5mm, CXR 4.1) proceed with the TB screening algorithm.
*TB High Risk Conditions:
- Clients who have been in close contact with an active TB case within the previous 5 years or during IME processing
- Client with HIV positive serology
- Client with a history of certain cancers originating in the head/neck region within the last 5 years (i.e. cancer of the oral cavity, salivary glands, nasal cavity or paranasal sinuses) NOTE: Thyroid Cancers are NOT considered high risk.
- Clients with advanced chronic renal failure or end-stage kidney disease (eGFR of <30 ml/min at any time during the IME)
- Clients with a solid organ or bone marrow transplant on immunosuppressant therapy. NOTE: immunotherapy without transplant is not to be included in this risk group at the moment.
Appendix A – Predictors of Active Pulmonary Tuberculosis
Symptoms
- Persistent cough
- Fever
- Night sweats
- Anorexia
- Fatigue
Signs
- Bronchial breathing, rales or crepitation
- Weight loss
- Hemoptysis
- Fibrotic lesion on chest x-ray
Risk Factors
- Country of origin with high TB incidence15
- Medical conditions affecting Immune System
- Extra Pulmonary Disease
- HIV infection4
- Malnutrition4
- Work environment with silica exposure13
Definition of Close Contact16
A TB close contact is an individual who has shared the same air space for a prolonged period of time with a person with infectious TB. The exact duration of exposure is traditionally at least 8 hours of cumulative exposure.
Examples of close contacts may include individuals:
- living in the same household
- sharing a confined workplace
- sharing sleeping quarters for at least one night
- living in residential institutions such as
- military barracks
- correctional institutions
- boarding schools
Appendix B – Sputum Collection/Induction
Specimen Comment Spontaneous Sputum - Adequate specimen and not saliva
- Minimum 5 ml
Induced Sputum - Can be used as of 3 years old
- Under medical supervision /approval according to standard procedure.
- Inhalation of 3% hypertonic saline with ultrasonic nebulizer
- Rate of 5-6 ml per minute
- Assess every 5 minutes and terminate when sputum obtained or 15 minutes of nebulisation is reached
Technical Instruction for all specimen types14
- Collection in morning under direct supervision and at least 1 hour between specimen
- Distilled or filtered bottle only for rinsing mouth
- Collection container: sterile, single use, screw capped 20 to 50 ml centrifuge tube
- Centrifugation required before preparing smears
- Identification: each specimen identified with unique bar code/number, date/time, specimen information
- Requisition: clearly mark sputum spontaneous or induced
- Transport: same day delivery. If not possible to deliver immediately to laboratory, refrigerate (2-8°C) using a refrigerator or cooler with ice packs
Procedures to be performed in designated collection area by trained technician using protective equipment (adequate respiratory protection with N-95 mask and gloves).
Initial TB investigation consists of three sputum specimens to undergo smear microscopy for acid-fast bacilli (AFB) as well as culture for Mycobacteria at the M. tuberculosis complex level for all three specimens. When available, molecular testing for Mycobacterium tuberculosis (MTB) based on nucleic acid amplification (NAAT) should be performed on the first specimen when all AFB smears are negative OR on one of any specimen with a positive smear2,6. Note that this test is not accepted as a substitute for tuberculosis cultures, which are required in all cases where sputum is collected.
The 3 sputum specimens can be collected on the same day at least 1 hour apart. Preferably spontaneously produced deep cough sputum should be obtained. When not possible to obtain spontaneous sputum, it is recommended that sputum induction be performed.2
Concentrated sputum smear microscopy using auramine stain with fluorescence microscopy is preferable, but Zielh-Neelsen or Kinyoun staining is acceptable.2 Solid and liquid medium cultures are required for every specimen sent for smear microscopy.7 Drug susceptibility test (DST) using phenotypic method should be performed for all first positive culture.1
References
- Immigration and Refugee Protection Act (A.C. 2001, c27), Part 1, Division 2.0, Sect 16(1)(2)(b)
- Canadian Tuberculosis Standards 7th Edition: 2014
- WHO Guidelines on Tuberculosis
- WHO: TB comorbidities and risk factors
- Canadian Panel Physician’s handbook
- Centers for Disease Control (CDC): Updated Guidelines for the Use of Nucleic Acid Amplification Tests in Diagnosis of Tuberculosis. MMWR Morb Mortal Wkly Rep.
- ATS/IDSA/CDC and Prevention Clinical Practice Guidelines: Diagnosis of tuberculosis in Adults and Children pg. e3 (PDF, 3.87 MB)
- Australia, CDNA National Guidelines for Public Health Units- Management of TB
- United Kingdom, NICE guideline for diagnosis and management of tuberculosis
- Center for Disease Control and Prevention, Tuberculosis treatment guidelines
- WHO guidelines for treatment of drug-susceptible tuberculosis and patient care (2017 update)
- WHO treatment guidelines for drug-resistant tuberculosis (2016 update) (PDF, 396 KB)
- Systematic screening for active tuberculosis: an operational guide by WHO (2015) (PDF, 6.74 MB)
- Mycobacteriology Laboratory Manual (PDF, 2.63 MB)
- High burden country list (TB- World Health Organisation) (PDF, 3.86 MB)
- WHO: Recommendations for Investigating Contacts of Persons with Infectious Tuberculosis in Low and Middle Income Countries pg. 28, 29 (PDF, 1.01 MB)
Appendix V: Training
Page details
- Date modified: