Antibiotic prescribing preceding COVID-19

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 48-4, April 2022: First Nations Health
Date published: April 2022
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 48-4, April 2022: First Nations Health
Surveillance
Antibiotic prescribing for respiratory tract infection across a national primary care network in 2019
Sabrina Wong1, Shan Rajapakshe2, David Barber3, Andrea Patey4, Wendy Levinson5, Rachael Morkem3, Gillian Hurwitz5, Kimberly Wintermute6, Jerome A Leis7,8
Affiliations
1 University of British Columbia Centre for Health Services and Policy Research and School of Nursing, Vancouver, BC
2 Island Medical Program, Faculty of Medicine, University of British Columbia, Victoria, BC
3 Department of Family Medicine, Queen's University, Kingston, ON
4 Ottawa Hospital Research Institute, Ottawa, ON
5 St. Michael's Hospital, Toronto, ON
6 North York General Hospital, Toronto, ON
7 Sunnybrook Health Sciences Centre, Toronto, ON
8 Division of Infectious Diseases and Centre for Quality Improvement and Patient Safety, Department of Medicine, University of Toronto, Toronto, ON
Correspondence
Suggested citation
Wong ST, Rajapakshe S, Barber D, Patey A, Levinson W, Morkem R, Hurwitz G, Wintermute K, Leis JA. Antibiotic prescribing for respiratory tract infection across a national primary care network in 2019. Can Commun Dis Rep 2022;48(4):157–63. https://doi.org/10.14745/ccdr.v48i04a06
Keywords: antimicrobial stewardship, primary care, audit and feedback, respiratory tract infection, validation
Abstract
Background: Respiratory tract infection (RTI) is the leading reason for avoidable antimicrobial use in primary care, yet provider-level feedback on its use is only available in some provinces. The aim of this study was to validate case definitions for RTI across the Canadian Primary Care Sentinel Surveillance Network (CPCSSN) and determine baseline provider-level variability in antimicrobial prescribing in 2019.
Methods: The RTI case definitions were developed using demographic, diagnostic coding and keywords in electronic medical record. Manual chart abstraction was performed to identify cases of acute otitis media. Remaining RTI definitions were validated using a random sample of 5,164 patients with encounters in 2019. The proportion of patients with an RTI treated with antibiotics was determined by provider, per patient, per episode and per patient encounter.
Results: Negative predictive value, positive predictive value and prevalence were as follows: 1.00 (0.99–1.00), 0.99 (0.96–0.99) and 4.14% (4.10–4.19) for common cold; 1.00 (0.99–1.00), 0.94 (0.88–0.98) and 1.09% (1.07–1.12) for acute otitis media; 0.98 (0.96–1.00), 0.93 (0.87–0.97) and 1.2% (1.18–1.22) for acute pharyngitis; 0.99 (0.99–1.00), 0.88 (0.81–0.93) and 1.99% (1.96–2.02) for sinusitis; 0.99 (0.97–0.99), 0.95 (0.89–0.98) and 4.01% (3.97–4.05) for acute bronchitis/asthma. By provider, median (interquartile range [IQR]) proportion treated with antibiotics (per patient) was 6.72 (14.92) for common cold, 64.29 (40.00) for acute otitis media, 20.00 (38.89) for pharyngitis, 54.17 (38.09) for sinusitis, 8.33 (20.00) for acute bronchitis/asthma and 21.10 (20.56) for overall RTI.
Conclusion: The CPCSSN can provide national surveillance of antimicrobial prescribing practices for RTI across primary care. Baseline variability underscores the need for provider feedback and quality improvement.
Introduction
Antimicrobial resistance has significant socioeconomic impacts in Canada, which are only expected to be magnified over the next decadeFootnote 1. Antimicrobial stewardship efforts to curb this trend has focused on hospitals, yet nearly 90% of antimicrobials are dispensed in the community sector, with a large proportion of these prescriptions arising from primary careFootnote 2.
Respiratory tract infection (RTI) is the leading cause of avoidable antimicrobial use in primary careFootnote 2Footnote 3. A national campaign led by Choosing Wisely Canada has developed prescriber-led practice changes and clinical tools to help facilitate avoidance of antibiotics in the management of RTIFootnote 4Footnote 5. One key challenge is that many primary care providers have never received feedback on their antimicrobial prescribing for RTI and may not recognize the need to make practice changes.
Accurate measurement of antimicrobial prescribing practices by primary care providers has been challenging in Canada due to the lack of a national antimicrobial surveillance system. While some provinces are already providing feedback to prescribersFootnote 6, the only large-scale data available regarding antibiotic use for RTI across Canada is an estimate based on population-based health services research, which is not available across all provincesFootnote 2.
The Canadian Primary Care Sentinel Surveillance Network (CPCSSN) is a national network of primary care clinics representing over two million patients and 1,500 primary care clinicians across eight provinces and one territoryFootnote 7. Each participating sentinel contributes electronic medical record (EMR) data to their respective network and the pan-Canadian data repository for the purposes of public health surveillance, quality improvement and research. Case definitions that incorporate keywords from EMRs have already been validated, which allows CPCSSN to generate surveillance on a wide range of diseasesFootnote 8Footnote 9Footnote 10. We hypothesized that CPCSSN would be ideally suited to accurately measure RTI in primary care as well as provider-level antimicrobial prescribing practices. If successful, this approach could in turn be used to generate provider feedback across CPCSSN based on peer comparison, which is known to improve antimicrobial prescribing practices in primary careFootnote 6Footnote 11. We undertook the following study to validate case definitions for RTI across a sample of CPCSSN sites and determine baseline provider-level variability in antimicrobial prescribing in the year preceding the coronavirus disease 2019 (COVID-19) pandemic.
Methods
Data source
Point-of-care de-identified data are extracted from the EMRs semiannually and transformed to a standard CPCSSN schema to form a regional and pan-Canadian data repository. The CPCSSN extracts clinical primary care data from 11 different EMR systems. Each EMR system has a different architecture and, even within one EMR system, may also have province-specific differences in the structure of the database where medical information is stored. As such, the transformation from EMR to the CPCSSN data repository includes advanced data cleaning and coding techniques. The architecture and approach have been previously described, including data flow, quality, mapping, cleaning and de-identificationFootnote 12. This project uses pan-Canadian data extracted from January 1 to December 31, 2019. Data included socio-demographics, providers, encounters, health conditions, risk factors, biometrics, laboratory results, procedures, medications and referral informationFootnote 12. Research Ethics Board approval was obtained at the site where manual chart abstraction was performed (approval #20-0037), in addition to University of British Columbia research ethics board where the case definition was examined using manual chart reviews to a subset of the CPCSSN data (approval #H20-02722) and Queen's University (approval #6034400) in order to apply the case definition to the entire pan-Canadian repository.
Development of case definitions
Several steps were performed to develop and validate the RTI case definition. First, a team of clinicians and researchers from CPCSSN and Choosing Wisely Canada, including two family physicians and one infectious diseases physician, met virtually to create the five case definitions (Table 1) that make up the majority of RTIs. Like previous workFootnote 1, these case definitions were primarily based on International Classifications of Diseases (ICD-9) codes found in EMRs. In addition to the ICD-9 codes, a set of related keywords, which could be found in a patient's record, was also included. These keywords were utilized to improve the specificity of the case definitions. The case definitions were modified and iterated upon until consensus was reached amongst the team members. Table 1 provides the final case definitions of the five RTI syndromes.
| Syndrome | ICD-9 codes for inclusion | Chart audit keywords | Exclusion (i.e. ICD-9 subcodes, keywords, etc.) | Population at risk |
|---|---|---|---|---|
| Acute otitis media (6 months of age or older) |
381: Eustachian tube disorders/otitis media, serous 382: Otitis media, suppurative |
Otitis media, AOM, otitis, acute otitis media | Chronic suppurative otitis media 381.6: Obstruction of eustachian tube 381.7: Patulous Eustachian tube 381.8: Other disorders of eustachian tube 381.9: Unspecified eustachian tube disorder |
17 years or younger |
| Uncomplicated pharyngitis | 034: Streptococcal sore throat/scarlet fever 463: Acute tonsillitis 464: Acute laryngitis, tracheitis, croup, epiglottis 462: Acute pharyngitis |
Pharyngitis, streptococcal throat, URI, URTI, viral URI, viral infection, viral URTI, laryngitis, bacterial pharyngitis, croup, tracheitis, epiglottis, acute laryngitis, acute tracheitis, acute laryngotracheitis | Abscess (peritonsilar, nasopharygneal, etc.), mononucleosis | All ages |
| Uncomplicated sinusitis | 461: Acute sinusitis | Uncomplicated sinusitis, bacterial sinusitis, viral sinusitis, sinusitis, maxillary, sinusitis, frontal, sinusitis, ethmoidal, sinusitis, sphenoid, sinusitis, other, sinusitis, unspecified | 473: Chronic sinusitis | All ages |
| Common cold | 460: Upper respiratory infection/nasopharyngitis, acute/pharyngitis/upper respiratory infection/acute nasopharyngitis (common cold) | Upper respiratory tract infection, URTI, cold, common cold, viral pharyngitis, nasopharyngitis, acute nasopharyngitis | N/A | All ages |
| Acute bronchitis/asthma (i.e. chronic lung condition exacerbations) | 466: Acute bronchitis 491: Chronic bronchitis 492: Emphysema 493: Asthma, allergic bronchitis 496: Other COPD |
Bronchitis, emphysema, must include COPD, chronic bronchitis, acute bronchitis, acute bronchiolitis, bronchitis, bronchiolitis | Must NOT include COPD (using the CPCSSN definition for COPD) 1. ICD-9 codes 490–492, 496 2. Problem list: bronchitis, emphysema, COPD/cold 3. Medication list: beta agonists, anticholinergics, inhalant corticosteroids 4. Risk factors: smoker |
All ages |
Abstraction of electronic medical records for cases of acute otitis media
A manual chart review of one RTI syndrome was completed at one CPCSSN site. Previous case validations have used manual charts review as a common standard of measurementFootnote 8Footnote 9Footnote 13; however, manually reviewing potentially thousands of charts is both resource intensive and time consumingFootnote 14. We chose to complete a manual chart review of otitis media because it was a specific definition with a well-defined population and required a small sample size. A standardized data collection form was created using a secure web-based Qualtrics survey (Qualtrics, Provo, Utah, United States) to ensure that a systematic approach was used to review the designated patients. The manual chart review was completed by one research team member who verified presence or absence of RTI for each patient by manually reviewing their EMR. A programmatic method, based on billing, encounter diagnosis information and age, of selecting patients for manual review was performed by a family physician at the selected clinic. A total of 418 patients representing 771 cases of otitis media were reviewed as part of this manual chart review. The chart review also included any further evidence of RTI by reviewing unstructured data (e.g. free text notes). The abstracted data were then reviewed by both the abstractor, the internist and the family physician to determine classification of RTI status.
Validation of other respiratory tract infection case definitions
To validate the remaining RTI definitions, a random sample of 5,164 patients from the pan-Canadian CPCSSN dataset was selected. The case definition was then applied and estimates of the prevalence of the five conditions were obtained. To ensure that these cases were correctly identified, a minimum of 100 random cases of each condition were selected, as well as a minimum of 100 cases with none of the five conditions, for additional database review by a blinded abstractor, as per the methodology described by Williamson et al.Footnote 9. Finally, we applied the resulting definitions to the pan-Canadian CPCSSN 2019 dataset.
Antibiotic prescribing associated with respiratory tract infection syndromes
Following validation of RTI syndromes, we examined the proportion of patients with an RTI that received an antibiotic prescription. The sample was restricted to all patients who had a visit in 2019 and had a recorded birth year and gender. No limit was applied to the number of RTI diagnoses included per patient over the study period. An RTI case was considered "treated" if the patient received a prescription, on the same day or within one day of the RTI diagnosis, for any medication typically used to treat RTI including penicillin VK, amoxicillin, amoxicillin-clavulinic acid, cefuroxime, cefaclor, cefadroxil, clarithromycin, azithromycin, moxifloxacin and levofloxacin.
Statistical analysis
To properly power the case definition validation, sample size calculations were performed. Sample size calculations were set to a precision of 0.10. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated using 2x2 tables comparing each of the constructed case definitions (case/no case) with the chart review diagnosis (case/no case). We constructed 95% confidence intervals (CI) for each parameter using the Clopper-Pearson approach for proportions. Since we were examining data across the pan-Canadian CPCSSN, we considered all measures greater than 80% to be acceptable. Summary data were tabulated for all RTI, as well as by each of the five clinical syndromes. The proportions were reported by patient, encounter and by episode. The proportion of patients with an RTI was tabulated by counting any patient with at least one RTI in 2019, out of all patients with at least one billing record in 2019. The proportion of patients treated was determined by counting a patient as "treated" if they had an associated antibiotic prescription on the same day or within one day of meeting the case criteria for an RTI, out of all the patients with at least one RTI in that year. The proportion of encounters with an RTI was tabulated by counting all encounters (unique date) that met the criteria for an RTI case in 2019, out of all encounters (defined as at least one billing on a unique day) in 2019. The proportion of RTI encounters treated was determined by counting an RTI case as "treated" if the case was associated with an antibiotic prescription, out of all the RTI cases in that year. If a patient's RTI case indicator (unique billing or encounter date) was more than 31 days from a previous RTI case indicator it was classified as a unique episode. The proportion of RTI episodes treated per individual provider was tabulated by counting all episodes of an RTI as "treated" if the episode was associated with an antibiotic prescription, out of all RTI episodes in that year. All data were analyzed in SAS version 9.4 (SAS Institute Inc., Cary, North Carolina, United States).
Results
For otitis media, among 418 patients manually reviewed to assess performance characteristics of the algorithm, 399 (95%) were confirmed to have acute otitis media while 19 (5%) did not. The algorithm correctly identified 392 (98%) cases and 15 (79%) patients without the infection. Table 2 summarizes the performance characteristics of the algorithm for acute otitis media.
| Performance characteristic | Detection of acute otitis media | 95% CI |
|---|---|---|
| Sensitivity | 0.98 | 0.96, 0.99 |
| Specificity | 0.79 | 54.43, 93.95 |
| PPV | 0.99 | 0.98, 1.00 |
| NPV | 0.68 | 0.50, 0.82 |
Table 3 presents the performance characteristics of all five RTI syndromes based on random sampling of pan-Canadian CPCSSN database. In this random sample of 5,164 patients, 2,981 (57.7%) were female and the median age was 44.7 years. When the case definitions were applied to the entire national CPCSSN database, we found that, of the 873,180 patients that visited their primary care provider in 2019, 11.33% (95% CI, [11.27, 11.40]) were diagnosed with an RTI. Evaluating each syndrome individually, we found the following prevalence (per patient): otitis media, 1.09% (95% CI, [1.07, 1.12]); pharyngitis, 1.20% (95% CI, [1.18, 1.22]); sinusitis 1.99% (95% CI, [1.96, 2.02]), common cold, 4.14% (95% CI, [4.10, 4.19] and acute bronchitis/asthma, 4.01% (95% CI, [3.97, 4.05]).
RTI syndrome |
Number of cases sampled | Sensitivity | Specificity | Negative predictive value | Positive predictive value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | 95% CI | n | 95% CI | n | 95% CI | n | 95% CI | |||
| Common cold | 172 | 1.00 | 0.98, 1.00 | 0.99 | 0.99, 0.99 | 1.00 | 0.99, 1.00 | 0.99 | 0.96, 0.99 | |
| Acute otitis media | 122 | 1.00 | 0.97, 1.00 | 0.99 | 0.98, 0.99 | 1.00 | 0.99, 1.00 | 0.94 | 0.88, 0.98 | |
| Acute pharyngitis | 122 | 0.88 | 0.81, 0.93 | 0.99 | 0.97, 0.99 | 0.98 | 0.96, 0.99 | 0.93 | 0.87, 0.97 | |
| Acute sinusitis | 121 | 0.99 | 0.95, 1.00 | 0.98 | 0.96, 0.99 | 0.99 | 0.99, 1.00 | 0.88 | 0.81, 0.93 | |
| Acute bronchitis/asthma | 121 | 0.93 | 0.88, 0.97 | 0.99 | 0.98, 1.00 | 0.99 | 0.97, 0.99 | 0.95 | 0.89, 0.98 | |
Evaluating the data per encounter, we found that, of the 3,747,610 encounters (identified by a unique date) in 2019, 3.52% (95% CI, [3.50, 3.54]) were diagnosed with an RTI. Evaluating each syndrome individually, we found the following prevalence (per encounter): otitis media, 0.35% (95% CI, [0.34, 0.35]); pharyngitis, 0.32% (95% CI, [0.32, 0.33]); sinusitis 0.56% (95% CI, [0.55, 0.57]), common cold, 1.16% (95% CI, 1.15, 1.17], acute exacerbation of chronic obstructive pulmonary disease, 1.32% (95% CI, [1.31, 1.33]). Figure 1 depicts the proportion prescribed an antibiotic per patient, per encounter, and per episode, across the five upper respiratory tract infection syndromes.
Figure 1: Variability in antibiotics prescribing in primary care for different upper respiratory tract infection syndromes per patient, per episode and per patient encounter

Text description: Figure 1
The graph depicts the proportion prescribed an antibiotic per patient, per encounter, and per episode, for five upper respiratory tract infection syndromes, across a national primary care network during 2019. There was significant variability identified for each syndrome with a median and interquartile range (IQR) of 64.29 (40.00) for acute otitis media, 20.00 (38.89) for uncomplicated pharyngitis, 6.72 (14.92) for common cold, 54.17 (38.09) for uncomplicated sinusitis, 8.33 (20.00) for acute bronchitis/asthma and 21.10 (20.56) for overall respiratory tract infection syndromes.
Figure 2 shows the proportion of antibiotics prescribed per patient at the prescriber level across CPCSSN. There was significant variability identified for each syndrome with a median and interquartile range (IQR) of 64.29 (40.00) for acute otitis media, 20.00 (38.89) for uncomplicated pharyngitis, 6.72 (14.92) for common cold, 54.17 (38.09) for uncomplicated sinusitis, 8.33 (20.00) for acute bronchitis/asthma and 21.10 (20.56) for overall RTI.
Figure 2: Antibiotic prescribing associated with different validated respiratory tract infection syndromes episodes by primary care provider, divided by quartileFigure 2 footnote a
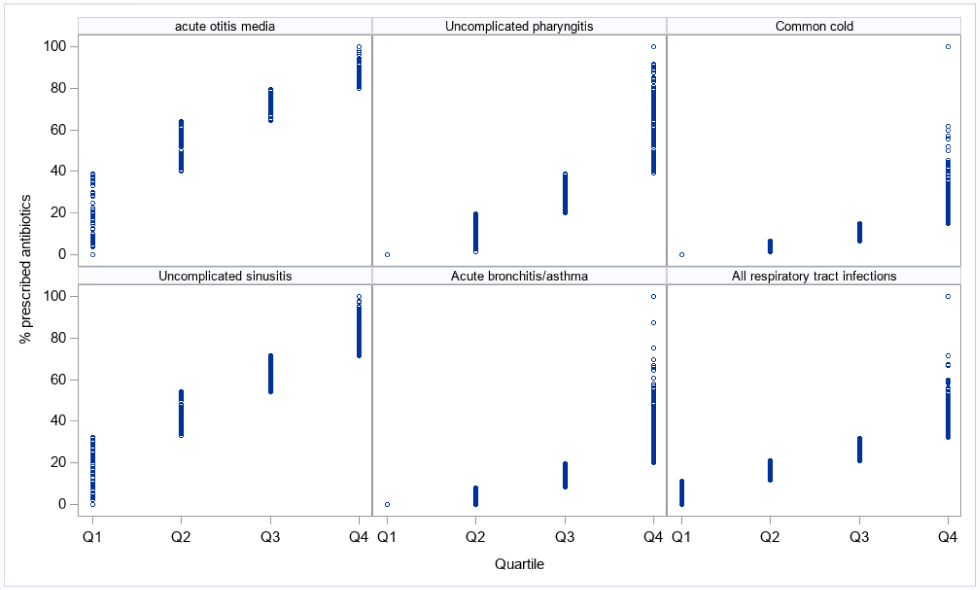
Text description: Figure 2
The graph shows the proportion of antibiotics prescribed per episode at the prescriber level across Canadian Primary Care Sentinel Surveillance Network (CPCSSN). The first-quartile (lowest antibiotic prescribers) prescribed antibiotics for less than 20% of respiratory tract infection syndrome episodes overall and never for common cold, uncomplicated pharyngitis and acute bronchitis/asthma. In contrast, the fourth-quartile (highest antibiotic prescribers) prescribed antibiotics to patients at a median of 22.22% for common cold, 57.14% for uncomplicated pharyngitis, 30.97% for acute bronchitis/asthma, 82.45% for uncomplicated sinusitis, 94.12% for acute otitis media, and 40.00% for overall respiratory tract infection syndrome episodes.
Discussion
This study found that CPCSSN can provide highly accurate surveillance for five common RTI syndromes across primary care. The variability in antibiotic prescribing practices identified underscores the need for feedback to providers and quality improvement as part of Canada's strategy to curb antimicrobial resistance.
Until now, surveillance of RTI and antibiotic prescribing practices in primary care has relied on provincial administrative databases that rely on physician billing claimsFootnote 3Footnote 6. Previous validation studies of physician RTI billing claims found a PPV that ranged between 0.84 and 0.96Footnote 15Footnote 16. In this study, we found that CPCSSN, which utilizes a combination of demographic factors, diagnostic codes and search terms in electronic medical records, similarly showed high PPV for surveillance of multiple different RTI case definitions.
Measuring antibiotic utilization in relation to RTI case definitions was assessed in different ways in our study. Antibiotic use per patient over the course of a year likely overestimated antibiotic prescribing, while antibiotic use per visit with RTI likely underestimated prescribing rates for patients with repeat visits. While the difference between these two approaches remained small, we found that antibiotic use per RTI episode, defined by incidence of a maximum of one RTI specific case definition per 30 days, fell between both measurements and may therefore provide the most accurate estimate of antibiotic prescribing practices.
Antibiotics for RTI are recognized to be the most common indication for unnecessary prescribing in primary care. Using our validated case definitions, we identified significant variability in antibiotic prescribing patterns with opportunity for improvement especially among those in the upper quartiles of antibiotic prescribing. Although our data do not directly measure appropriateness, this inter-provider variability in prescribing has been identified previously and was not explained by clinical patient differencesFootnote 2Footnote 3Footnote 17. In this study, prescribers in the fourth quartile (those who prescribe the most) were found to prescribe antibiotics for nearly 100% of episodes of otitis media and sinusitis, and over half of pharyngitis and common colds. While there are no established benchmarks, the prescribers in the top quartile had rates of prescribing rates of close to zero for the common cold and pharyngitis as would be expected, and less than 30% for sinusitis and otitis media.
To address high-volume prescribing in primary care, multiple prior randomized controlled trials have demonstrated that peer comparison and feedback can significantly curb antimicrobial useFootnote 6Footnote 11Footnote 18. A recent trial in Ontario found that mailing a single letter to primary care providers notifying them that they are among the highest quartile of antibiotic prescribers compared with their peers resulted in a 4.2% relative difference in overall ambulatory antibiotic prescribing and $1.7 million in drug cost savingsFootnote 6. Our validation of RTI case definitions across CPCSSN and identification of the high-volume prescribers will allow for similar targeted feedback interventions across this national primary care network.
Limitations
Our study has several important limitations. First, CPCSSN currently represents less than 10% of all primary care providers and therefore our findings may not represent antibiotic prescribing practices across Canada; however, greater representation may be possible in the future by scaling up the number of practices participating in this national primary care network. Second, the performance characteristics of our RTI case definitions vary by syndrome but the overall high PPV makes these data conducive to use for audit-and-feedbackFootnote 19. Finally, this study was conducted based on chart abstraction of cases prior to the COVID-19 pandemic which has greatly affected the incidence and management of RTIFootnote 20. Further follow-up will be required in the post-COVID-19 era to reassess the incidence of different RTI syndromes and antibiotic prescribing practices.
Conclusion
National surveillance of antimicrobial prescribing practices in the community will be a vital strategy for curbing antimicrobial resistance. Our validation study confirmed that CPCSSN can provide this surveillance for RTI, which is the most common reason for antibiotic prescriptions in primary care. Future studies should focus on feedback to high-volume prescribers at a national scale, in combination with clinical tools that support practice improvement.
Authors' statement
All authors contributed to the preparation of this manuscript.
The content and view expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
Competing interests
G Hurwitz, W Levinson and JA Leis receive support from Choosing Wisely Canada. No other competing interests to declare.
Acknowledgements
We thank J Queenan for assistance with sample size calculation.
Funding
Using Antibiotics Wisely, a campaign of Choosing Wisely Canada, is supported by Public Health Agency of Canada.
Page details
- Date modified:
