Understanding a broader range of opioid-related hospitalizations in Canada
The Public Health Agency of Canada, in collaboration with the provincial and territorial (PT) offices of Chief Coroners and Chief Medical Examiners, PT public health and health partners, and Emergency Medical Services data providers releases quarterly reports on apparent opioid-related deaths and Emergency Medical Services responses for suspected opioid-related overdoses. The Public Health Agency of Canada also collaborates with Health Canada to report on hospitalizations for opioid-related poisonings (overdoses) using hospital administrative data from the Canadian Institute for Health Information (CIHI).
However, harms related to opioids extend beyond overdoses and, in some cases, death. Administrative data from CIHI on hospitalizations can also be used to examine other types of opioid-related harms, including adverse drug reactions from prescribed opioids, and mental and behavioural disorders related to the use of opioids.
This brief report summarizes national data (excluding Quebec) for these three categories of hospitalizations for opioid-related harms, between April 1, 2018 to March 31, 2019. Each type of opioid-related harm is presented by sex and age group. Additionally, total length of stay (LOS) in hospital and what happened after being hospitalized (discharge disposition) is described for each type of harm.
Definitions of opioid-related harms included in this report
Opioid-related poisonings: Opioid poisoning harms (overdose) resulting from incorrect use of opioids in an intentional, accidental or unknown manner. Opioid poisonings may involve non-pharmaceutical opioids, pharmaceutical opioids, or both pharmaceutical and non-pharmaceutical opioids.
Pharmaceutical opioids refer to opioids that were manufactured by a pharmaceutical company and approved for medical purposes in humans. Pharmaceutical opioids can be obtained by a prescription, but sometimes may also be obtained through other means.
Adverse drug reactions from prescribed opioids: occurs when an opioid is taken as prescribed and results in harm, for example, delirium, confusion, and respiratory depression.
Opioid use disorders: includes mental health and behavioural disorders that are related to the use of opioids.
Overall rates by sex
Across Canada (excluding Quebec), overall rates of hospitalization for opioid-related harms were highest for opioid use disorders, followed by adverse drug reactions from prescribed opioids, and opioid-related poisonings. Hospitalizations for opioid-related poisonings (overdoses) and opioid use disorders were higher among males than females, while hospitalizations for adverse drug reactions from prescribed opioids were higher among females.

Text equivalent (Figure 1)
| Opioid-related harm hospitalization | Crude rate per 100,000 population for both sexes | Crude rate per 100,000 population for males | Crude rate per 100,000 population for females |
|---|---|---|---|
| Opioid-related poisonings | 17.7 | 19.9 | 15.5 |
| Adverse drug reactions from prescribed opioids | 21.6 | 17.9 | 25.2 |
| Opioid use disorders Footnote * | 35.1 | 38.9 | 31.5 |
|
|||
Rates by age and sex
Age and sex specific crude rates also varied by type of opioid-related harm. Similar to the pattern observed for apparent opioid-related deaths, younger adults had the highest rates of hospitalization for opioid-related poisonings. Younger males (ages 20 to 29 years, and 30 to 39 years) had the highest rates of hospitalizations for this category of harms. In contrast, rates for hospitalization for adverse drug reactions from prescribed opioids were concentrated among both males and females who were 60 years of age and older, with rates of 61 per 100,000 population and 75 per 100,000 population, respectively. In comparison, rates for all other age groups for adverse drug reactions from prescribed opioids by sex were 20 per 100,000 population or less. The distribution of rates for hospitalizations for opioid-use disorder were more similar to those for opioid-related poisonings; however, there was a more even pattern across the sexes - males and females had similar rates in each age group.

Text equivalent (Figure 2)
| Age group | Crude rate per 100,000 population for males | Crude rate per 100,000 population for females |
|---|---|---|
| 0 to 9 years | 2.2 | 1.7 |
| 10 to 19 years | 6.1 | 10.5 |
| 20 to 29 years | 27.9 | 17.4 |
| 30 to 39 years | 34.0 | 15.9 |
| 40 to 49 years | 23.8 | 18.3 |
| 50 to 59 years | 22.6 | 20.8 |
| 60 years and older | 18.0 | 17.7 |
| All ages | 19.9 | 15.5 |
'Other sex' are not reported as counts were less than 5. Source: Discharge Abstract Database, Canadian Institute for Health Information |
||

Text equivalent (Figure 3)
| Age group | Crude rate per 100,000 population for males | Crude rate per 100,000 population for females |
|---|---|---|
| 0 to 9 years | 3.5 | 3.2 |
| 10 to19 years | 2.5 | 3.8 |
| 20 to 29 years | 2.7 | 4.8 |
| 30 to 39 years | 3.2 | 8.2 |
| 40 to 49 years | 6.7 | 11.7 |
| 50 to 59 years | 16.0 | 20.4 |
| 60 years and more | 60.7 | 74.6 |
| All ages | 17.9 | 25.2 |
'Other sex' are not reported as counts were less than 5. Source: Discharge Abstract Database, Canadian Institute for Health Information |
||
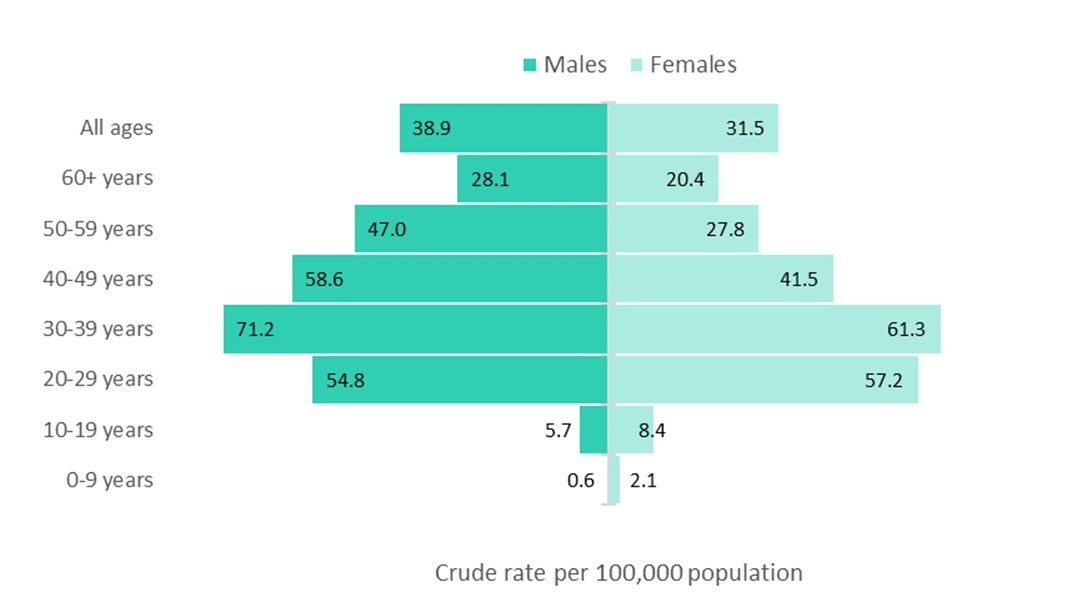
Text equivalent (Figure 4)
| Age group | Crude rate per 100,000 population for males | Crude rate per 100,000 population for females |
|---|---|---|
| 0 to 9 years | 0.6 | 2.1 |
| 10 to19 years | 5.7 | 8.4 |
| 20 to 29 years | 54.8 | 57.2 |
| 30 to 39 years | 71.2 | 61.3 |
| 40 to 49 years | 58.6 | 41.5 |
| 50 to 59 years | 47.0 | 27.8 |
| 60 years and more | 28.1 | 20.4 |
| All ages | 38.9 | 31.5 |
|
||
Length of stay
Length of stay in hospital varied by type of opioid-related harm. Median length of stay was longest for adverse drug reactions from prescribed opioids, at eight days, and shortest for opioid-related poisonings, at three days. Length of stay was similar for males and females across each of the harms included.

Text equivalent (Figure 5)
| Opioid-related harm hospitalization | Median total length of stay in days for males | Median total length of stay in days for females |
|---|---|---|
| Opioid-related poisonings | 3 | 3 |
| Adverse drug reactions from prescribed opioids | 8 | 8 |
| Opioid use disorders Footnote * | 5 | 6 |
|
||
Discharge disposition
Similarly, the distribution of discharge disposition varied by type of harm. For all types of opioid-related hospitalizations, most patients were discharged home, ranging from 60% to 65% for males, and 64% to 67% for females. Similar proportions of hospitalizations for opioid-related poisonings and patients hospitalized for adverse drug reactions from prescribed opioids indicated that the patient died (8% and 9% for males, and 5% each for females). The proportion of hospitalizations that indicated the patient died was almost twice as high for males compared to females, across all types of opioid-related harms. This is consistent with the disproportionate burden of apparent opioid-related deaths among males as compared to females. The proportion of patients leaving against medical advice demonstrated considerable variability: while 13% of males and 9% of females hospitalized for an opioid-related poisoning left against medical advice, as did 16% of males and 17% of females hospitalized for an opioid use disorder, only 2% of males and 1% of females hospitalized for an adverse drug reaction from prescribed opioids did so. Patients who leave against medical advice may not have received all of the medical care or supports available.

Text equivalent (Figure 6)
| Discharge disposition from hospital | Percent of opioid-related poisonings for males | Percent of opioid-related poisonings for females | Percent of adverse reactions to prescribed opioid for males | Percent of adverse reactions to prescribed opioid for females | Percent of opioid use disorders for malesFootnote * | Percent of opioid use disorders for femalesFootnote * |
|---|---|---|---|---|---|---|
| Transfer | 19% | 19% | 24% | 27% | 20% | 18% |
| Home | 60% | 67% | 65% | 66% | 63% | 64% |
| Leave | 13% | 9% | 2% | 1% | 16% | 17% |
| Died | 8% | 5% | 9% | 5% | 2% | 1% |
|
||||||
In summary
Understanding patterns of a range of opioid-related harms can help inform clinical and public health actions to address the opioid overdose crisis. These data demonstrate that not only are opioid-related poisonings (overdoses) a source of considerable morbidity for Canadians, there are a notable number of hospitalizations for adverse drug reactions to prescribed opioids, and for opioid use disorders. While younger adults are disproportionately represented among hospitalizations for opioid-related poisonings (overdoses) and opioid-use disorder, older adults are disproportionately affected by adverse drug reactions related to prescribed opioids. In addition, while most people hospitalized for any opioid-related harm are discharged home, a notable proportion of those hospitalized for opioid-related poisoning or opioid use disorders leave before being formally discharged. This may indicate a need to better understand the acceptability of health care for these conditions. Continuing to understand patterns of opioid-related harms through hospitalization and other data sources will help Canada address the continuing opioid overdose crisis.
Acknowledgements
We would like to acknowledge the Canadian Institute for Health Information (CIHI) for collecting and providing the data used for reporting opioid-related hospitalizations.
Disclaimer
Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed herein are those of the authors, and not necessarily those of the Canadian Institute for Health Information (CIHI).
Technical Notes
Definitions (Refer to Appendix A for full definition)
Length of stay: Represents the total length of stay in hospital (including the amount of time the patient received acute care and alternative level of care, if applicable).
Discharge disposition: Identifies the location where the patient was discharged to or the status of the patient on discharge from hospital.
Methodology
Data from CIHI's Discharge Abstract Database (DAD) for the fiscal year April 1, 2018 to March 31, 2019 was analysed for this report. This analysis was limited to acute inpatient hospitalizations, which are nationally representative across Canada, with the exception of Quebec. This analysis presents the number of acute inpatient hospitalizations for opioid-related harms, it does not reflect the number of patients who were hospitalized in the study year. It is possible some patients may have been hospitalized more than once for an opioid-related harm. Only crude rates are presented.
The International Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA) is used in the DAD to capture diagnoses from the patient's hospitalization. It is the national standard for reporting morbidity statistics. Refer to Appendix A for a complete listing of all ICD-10-CA diagnosis codes used to identify opioid-related harms presented in this report. More information on the DAD and ICD-10-CA coding can be found on CIHI's website.
For opioid-related poisoning and opioid use disorders, analyses were restricted to significant diagnosis types; hospitalizations in which the opioid-related harm was considered influential to the time spent in hospital and treatment received by the patient while there. For hospitalizations associated with an opioid-related poisoning and/or an opioid use disorder, the following types of diagnoses were retained for analysis:
- Most responsible diagnosis ("M")
- Pre-admit comorbidity ("1")
- Post-admit comorbidity ("2")
- Service transfer diagnosis ("W", "X", and "Y")
Adverse drug reactions from prescribed opioids are considered external cause of injury codes. In line with CIHI coding standards, a diagnosis type of "9" was used for identifying these records.
A diagnosis prefix of "Q", indicating unconfirmed diagnoses or query diagnoses recorded by the physician, were excluded from these analyses. Records indicating the patient was admitted to the facility as a cadaveric donor and still births were also excluded.
| Original Discharge Disposition field values | Recoded Discharge Disposition field values |
|---|---|
| Inpatient Care ('10') ED and Ambulatory Care ('20') Residential Care ('30') Group/Supportive Living ('40') Correctional Facility ('90') |
Transfer |
| Home with Support/Referral ('04') Private Home ('05') |
Home |
| Absent Without Leave (AWOL) ('61') Left Against Medical Advice (LAMA) ('62') Did not Return from Pass/Leave ('65') |
Leave |
| Died While on Pass/Leave ('66') Suicide out of Facility ('67') Died in Facility ('72') Medical Assistance in Dying (MAID) ('73') Suicide in Facility ('74') |
Died |
Crude rates for hospitalization for each opioid-related harm were calculated using census data for July 1, 2018 from Statistics Canada.
Limitations
General notes
- 1. Hospitalizations for opioid use disorders are underrepresented in this report as the data source used (Discharge Abstract Database) does not include full coverage for hospitalizations due to mental illness and substance use disorders. Additional opioid use disorder hospitalizations may be captured in the Ontario Mental Health Reporting System (OMHRS) and therefore these results should be interpreted with caution.
- 2. Due to changes in the field values implemented April 1, 2018 (applicable to discharge disposition), results are presented by fiscal year as opposed to calendar year.
- 3. It is possible for a patient to have a diagnosis of an opioid-related poisoning, in addition to an opioid use disorder, on the same hospital record. Totals for the three categories cannot be summed to represent the overall number of hospitalizations for opioid-related harms.
- 4. The DAD captures patients discharged from hospital. Patients who were still hospitalized during the study year are not captured in this report.
- 5. Data released by provinces and territories may differ from the data provided in this report due to the availability of updated data, differences in the type of data reported, the use of alternate age groupings, differences in time periods presented and/or population estimates used for calculations, etc.
Data on sex
- 6. In the DAD, data on sex is typically recorded based on biological determination or legal documentation. Although 'other' sex group is available, the counts were too low to include in this report. Therefore, 'other' sex group was retained in overall analyses, but were excluded from all analyses by sex to avoid disclosure.
Data suppression
Counts less than 5 are suppressed according to CIHI's privacy guidelines.
Appendix A
| Type of Opioid-Related Harm | ICD-10-CA Code | Description |
|---|---|---|
| Opioid-related poisonings | T40.0 | Poisoning by opium |
| T40.1 | Poisoning by heroin | |
| T40.2 | Poisoning by other opioids | |
| T40.20 | Poisoning by codeine and derivatives | |
| T40.21 | Poisoning by morphine | |
| T40.22 | Poisoning by hydromorphone | |
| T40.23 | Poisoning by oxycodone | |
| T40.28 | Poisoning by other opioids not elsewhere classified | |
| T40.3 | Poisoning by methadone | |
| T40.4 | Poisoning by other synthetic narcotics | |
| T40.40 | Poisoning by fentanyl and derivatives | |
| T40.41 | Poisoning by tramadol | |
| T40.48 | Poisoning by other synthetic narcotics not elsewhere classified | |
| T40.6 | Poisoning by other and unspecified narcotics | |
| Adverse drug reactions from prescribed opioids | Y45.0 | Opioids and related analgesics |
| Y45.01 | Codeine and derivatives | |
| Y45.02 | Morphine | |
| Y45.03 | Hydromorphone | |
| Y45.04 | Oxycodone | |
| Y45.05 | Fentanyl and derivatives | |
| Y45.06 | Tramadol | |
| Y45.09 | Other and unspecified opioids and related analgesics | |
| Opioid use disorders | F11.0 | Mental and behavioural disorders due to use of opioids, acute intoxication |
| F11.1 | Mental and behavioural disorders due to use of opioids, harmful use | |
| F11.2 | Mental and behavioural disorders due to use of opioids, dependence syndrome | |
| F11.3 | Mental and behavioural disorders due to use of opioids, withdrawal state | |
| F11.4 | Mental and behavioural disorders due to use of opioids, withdrawal state with delirium | |
| F11.5 | Mental and behavioural disorders due to use of opioids, psychotic disorder | |
| F11.6 | Mental and behavioural disorders due to use of opioids, amnesic syndrome | |
| F11.7 | Mental and behavioural disorders due to use of opioids, residual and late- onset psychotic disorder | |
| F11.8 | Mental and behavioural disorders due to use of opioids, other mental and behavioural disorders | |
| F11.9 | Mental and behavioural disorders due to use of opioids, unspecified mental and behavioural disorder |
Page details
- Date modified: