Caring for Canadians: Canada’s Future Health Workforce – The Canadian Health Workforce Education, Training and Distribution Study
Download in PDF format
(2.9 MB, 24 pages)
Organization: Health Canada
Date published: 2025-01-30
Cat.: H22-4/42-2025E-PDF
ISBN: 978-0-660-74277-9
Pub.: 240617
Executive summary
Note: This is a summary of the report. To receive a copy of the full report, send a request to: hhr-rhs@hc-sc.gc.ca.
On this page
Introduction
The Canadian Health Workforce Education, Training and Distribution Study (the Study), the first pan-Canadian study of its kind, confirms a significant gap in the health workforce that, if no action is taken, will worsen over ten years. The Study highlights the even larger gaps in rural and remote communities, the limited training capacity in the North and the unique challenges of building the Indigenous workforce. An important interdependence exists between provincial and territorial jurisdictions and Indigenous partners such that addressing health workforce challenges can only occur with collaboration across the country.
Health professional education and training capacity must increase now. Moving forward, Canada must establish the ability to plan with a strong foundation of data on health professionals in training and in the workforce; integrated health workforce modelling; a health professions education and workforce planning collaborative council including representation from ministries of health and education and Indigenous partners; and engagement with educators, regulators, accreditors, employers, certification bodies and health professions associations to enable the changes required to address the health care needs of the populations of Canada.
Background
In October 2023, federal, provincial, and territorial (FPT) Health Ministers except Quebec, requested a study to better understand how they can address the domestic supply of health workers. Caring for Canadians: Canada’s Future Health Workforce - The Canadian Health Workforce Education, Training and Distribution Study (the Study) has offered an important opportunity to take stock of Canada’s capacity to produce a domestic supply of key health professionals, to leverage current pan-Canadian data and tools to project future supply and demand for the health workforce and find a way forward in bridging the gap. Note: Quebec does not subscribe to pan-Canadian approaches regarding the health workforce and intends to retain its full autonomy in its jurisdiction in the administration of its health system.
The Study’s terms of reference were approved by the Conference of Deputy Ministers in January 2024. The scope of the study includes five professions engaged in primary care for which health workforce information was available from the Canadian Institute for Health Information (CIHI), including nursing (licensed practical nurses, registered psychiatric nurses, registered nurses and nurse practitioners), occupational therapy, physiotherapy, pharmacy and physicians (with a specific focus on family medicine). Data on these health professions was collected from provincial and territorial governments, health profession faculty associations and CIHI. Modelling of the available pan-Canadian data was used to estimate the current and projected workforce supply of, and demand for, the health professions. The Study also considers strategies and initiatives to support the inclusion, recruitment, and retention of Indigenous Peoples in the health workforce. This work was undertaken by Karhinéhtha´ Cortney Clark, a Mohawk woman from Wáhta Mohawk Territory, and Indigenous health researcher.
Study oversight was carried out by the FPT Committee on Health Workforce (CHW) and an FPT Project Team consisting of four provincial and territorial (PT) representatives, CIHI, Health Workforce Canada (HWC), and Health Canada, and was chaired by Dr. Geneviève Moineau, Chief Medical Workforce Advisor. CHW approved the data requests sent to national educational organizations and PT ministries of health. Simultaneously, the Project Team updated a health workforce projection model (CIHI’s Physician Resource Planning Tool) and created a new model (Health Canada’s Pan-Canadian Health Workforce Projection Model).
Dozens of engagements were undertaken with Indigenous partners, health workforce scholars and experts, national leaders of organizations for each profession, health profession education leaders and innovators, and representatives from various ministries of health across the country to seek advice on the proposed data sources, tools and models, methods and assumptions, literature on workforce supply and demand projections modelling, and to learn about current innovations in education.
The Study had an ambitious timeline based on the request to report back to Ministers at the fall 2024 Health Ministers’ meeting. The full Study report includes an introduction to the Study, to health professions education and to the data sources used. It also includes considerations to support an Indigenous health professions workforce, developed by an Indigenous health researcher. This is followed by the methodology, current state analysis, challenges and barriers, innovations and workforce supply demand and gap projections chapters. The Study closes with reflections, recommendations, and future considerations.
Findings
Indigenous health workforce education, training and distribution
First Nations, Inuit and Métis Peoples experience significant disparities and challenges in accessing health professions education and training opportunities in Canada. Rooted in historical injustices and ongoing systemic barriers, these issues necessitate urgent action to foster a culturally safe and more culturally informed health workforce. Indigenous health workers are critical to the creation of a culturally safe environment for Indigenous Peoples seeking health care and to helping address important health workforce gaps. The roles of Indigenous health helpers, such as Elders and Knowledge Keepers, must be considered. Indigenous-led solutions addressing health education, training and workforce development should address gaps while aligning with the Truth and Reconciliation Commission’s Calls to Action,Footnote 1 the United Nations Declaration on the Rights of Indigenous PeoplesFootnote 2 and regional Indigenous-led data collection and reporting.
Health professions education and training data
An overview of the available education programs in Canada for the selected health professions, including the national program capacity and number of institutions, is available in Table 1.
| Professionals | Program capacityTable 1 Footnote a | Number of institutionsTable 1 Footnote b | Number of provinces and territories offering the education program | |
|---|---|---|---|---|
| NursesTable 1 Footnote c | Licensed Practical Nurses | NR | 69 | 13 |
| Registered Psychiatric Nurses | NR | 6 | 4 | |
| Registered Nurses | NR | 77 | 12 | |
| Nurse Practitioners | NR | 24 | 10 | |
| Occupational Therapists | 1,339 | 14 | 7 | |
| Physiotherapists | 1,302 | 15 | 7 | |
| PharmacistsTable 1 Footnote d | 1,436 | 10 | 8 | |
| Physicians | MD program | 3,005 | 17 | 8 |
| All medical residency positions | 3,393 | 17 | 8 | |
| Family medicine residency positions | 1,557 | 17 | 8 | |
|
||||
Obtaining the education and training data from most sources was very difficult. There were significant variations in the data collected from various sources and they also differed significantly by profession, even in the same jurisdiction. Some national health education organizations collected comprehensive data while others did not. Although information was available at the educational program level and could be collated by the national organizations, in some cases, such as for nursing, there was a reliance on PT health ministry partners to find the information on the four nursing categories under study. Most ministries of health had to then request the information from their ministry of education counterparts, which, for some, was challenging and time consuming.
There was significant missing data on the four nursing categories. Only the first-year enrolment, total number of students and total number of graduates were consistently provided. The inability to confirm program capacity information for nursing, Canada’s largest group of regulated health professionals, is of significant concern. Program capacity is essential information to support health workforce education planning. However, ministries of education may have had additional data that was not available for the purposes of the Study, due to time and resource constraints.
The Study also sought to understand the education and training environment of rural and remote populations. An attempt was made to obtain data on students’ place of residence at the time of entry to their educational program, training locations including rural and remote placements, and location of employment at graduation. Despite the Study’s best efforts, only the location of the programs was made available, with few exceptions (see Figure 1).
Figure 1. Number of education and training programs located in urban and rural or remote communities for select health professionals, 2022-2023
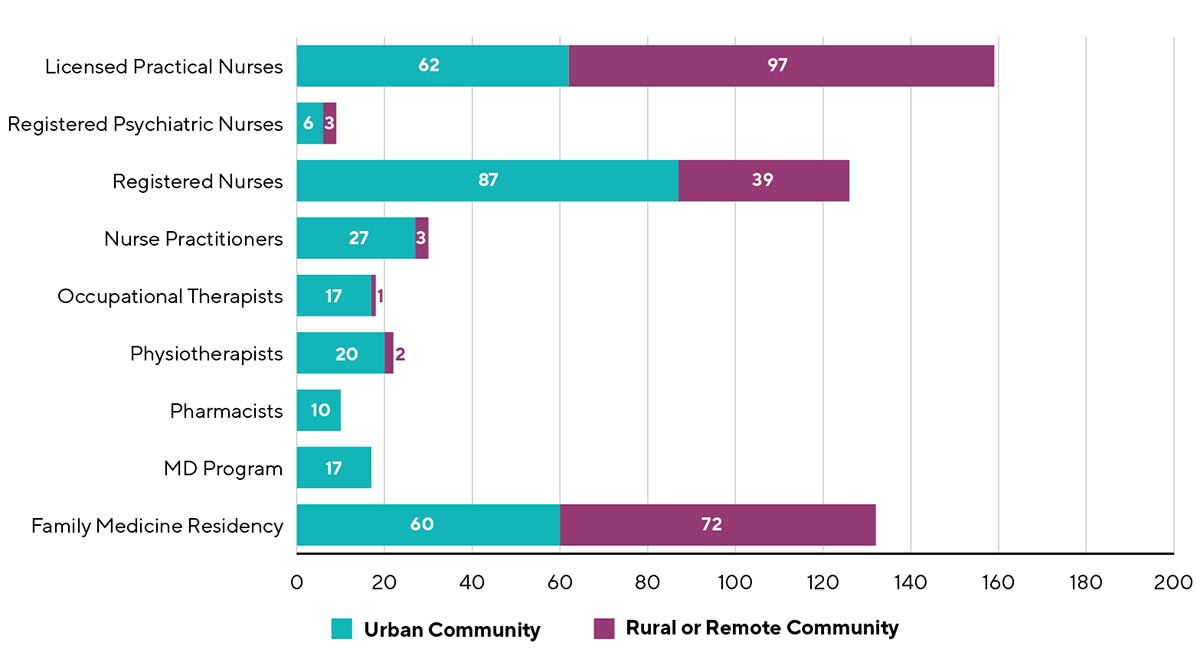
Figure 1 notes:
As Quebec considers its health workforce to be its exclusive responsibility, Quebec did not provide data for the Study. There were 29 family medicine residency programs with insufficient information to determine the type of community where the program was delivered.
Figure 1: Text description
Figure 1 represents a horizontal bar graph showing the number of programs located in urban and rural or remote communities, 2022 to 2023.
Number of education and training programs located in urban and rural or remote communities for select health professionals.
| Profession | Urban Community | Rural or Remote Community |
|---|---|---|
| Licensed Practical Nurses | 62 | 97 |
| Registered Psychiatric Nurses | 6 | 3 |
| Registered Nurses | 87 | 39 |
| Nurse Practitioners | 27 | 3 |
| Occupational Therapists | 17 | 1 |
| Physiotherapists | 20 | 2 |
| Pharmacists | 10 | 0 |
| MD Program | 17 | 0 |
| Family Medicine Residency | 60 | 72 |
The size of first year enrolment and graduation cohorts in the health professions studied is generally increasing at a slow pace, if at all, between 2018-19 and 2022-23. The number of graduates in physiotherapy, occupational therapy, pharmacy, licensed practical nurses (LPN), and registered psychiatric nurses (RPN) programs had 0-2% increase per year while family physicians had a 2.5% increase, and registered nurse (RN) programs had a 5% increase. The only significant increase noted was for nurse practitioners (NP) who had a 13% annual increase over four years. The COVID-19 pandemic years of 2020-22 caused some fluctuations in the data, however it was difficult to determine the extent of the impact on student enrolment. It is the Study’s assumption that the final set of data for 2022-23 shows minimal residual pandemic effect.
Although data on applications to nursing programs was not included in the Study due to variability in data collection, for all other professions, sufficient applications were received compared to the program capacity. When interpreting this data, it is important to consider that applications may be submitted to many programs and/or across programs and jurisdictions by the same individual.
Student withdrawals from programs were significant in all years for occupational therapy and physiotherapy programs with a rate of 9% and 8%, respectively. These data were not available for nursing programs; however, nursing programs are also impacted by withdrawals.Footnote 3 Leaders in occupational therapy and physiotherapy professions confirmed that the main reason for withdrawal from these programs was acceptance into medical school. Health professions education and workforce planners should take this mobility between programs into account when planning education program capacity to meet population needs.
Health workforce data and supply and demand for the current state, gap projections and scenario analyses
The current state (baseline) and projections results for the workforce supply, demand, and gap analyses reported are based on the best data available at the time of the Study. Efforts were made to ensure the data used, and how they were treated, were appropriate. This was done through a consultation process that sought agreement from health workforce and health professions education experts. Based on available data, as shown in Table 2, the average annual growth in the projected workforce supply from 2022 to 2034 ranges from 1.1% for pharmacists, 1.3% for RNs, 1.7% for occupational therapists, 1.8% for family physicians, 1.9% for LPNs, 2.0% for RPNs, 2.1% for physiotherapists, and 4.1% for NPs.
| Health occupation | Average annual growth rate (2022 to 2034) |
|---|---|
| Licensed Practical NurseTable 2 Footnote * | 1.9% |
| Registered Psychiatric NurseTable 2 Footnote * | 2.0% |
| Registered Nurse | 1.3% |
| Nurse Practitioner | 4.1% |
| Occupational therapist | 1.7% |
| Physiotherapist | 2.1% |
| PharmacistTable 2 Footnote * | 1.1% |
| Family physician | 1.8% |
|
|
Figures 2a and 2b provide the trends in the supply-demand gap for each health profession. Gaps increase over the 10-year study period for RNs, pharmacists and family physicians; they decrease for LPNs, RPNs, NPs, occupational therapists and physiotherapists.
Figure 2a. Base case workforce supply-demand gap, head counts, licensed practical nurses, registered nurses, and family physicians, Canada, 2022-2034
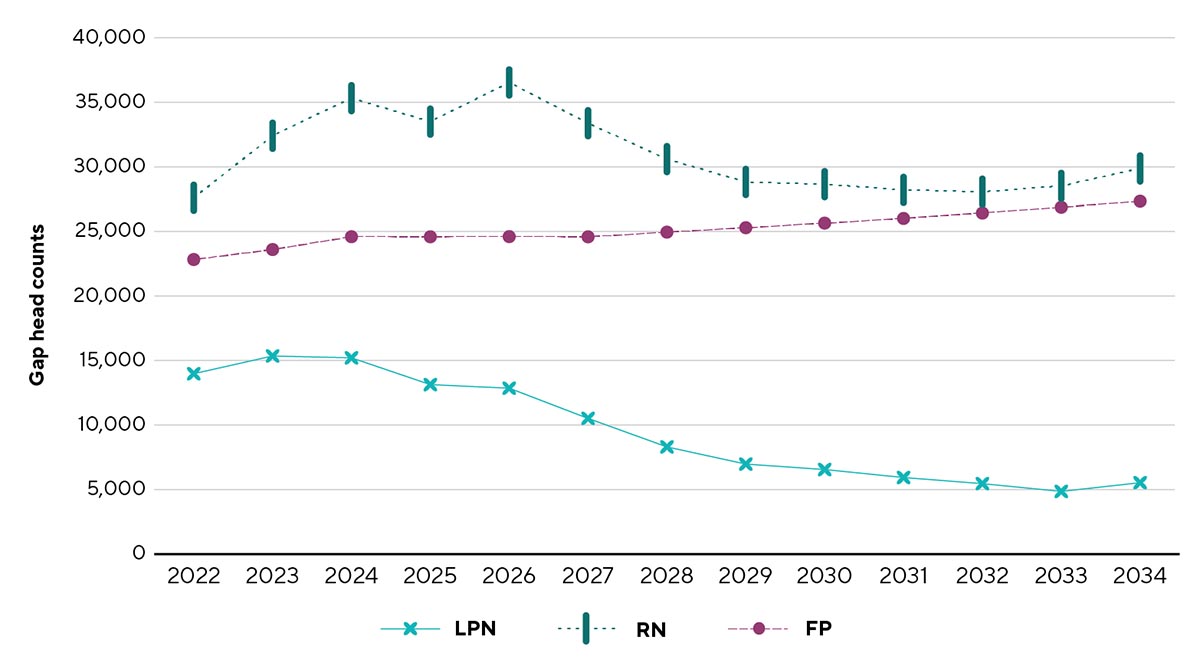
Figure 2a: Text description
Figure 2a presents a line graph illustrating the gap between supply and demand under the base case, in head counts, for licensed practical nurses, registered nurses and family physicians in Canada from 2022 to 2034.
| Year | LPN | RN | FP |
|---|---|---|---|
| 2022 | 13,976 | 27,608 | 22,823 |
| 2023 | 15,350 | 32,414 | 23,596 |
| 2024 | 15,207 | 35,326 | 24,591 |
| 2025 | 13,132 | 33,506 | 24,586 |
| 2026 | 12,855 | 36,542 | 24,600 |
| 2027 | 10,514 | 33,385 | 24,583 |
| 2028 | 8,306 | 30,605 | 24,946 |
| 2029 | 6,976 | 28,837 | 25,287 |
| 2030 | 6,553 | 28,662 | 25,642 |
| 2031 | 5,934 | 28,221 | 26,005 |
| 2032 | 5,460 | 28,078 | 26,422 |
| 2033 | 4,858 | 28,530 | 26,872 |
| 2034 | 5,533 | 29,878 | 27,344 |
LPN: licensed practical nurse; RN: registered nurse; FP: family physician. Source: Health Canada analysis using CIHI’s PRPT with adjustments and Health Canada’s pan-Canadian Health Workforce Projections Model. Family physician projection gaps are based on the scenario that is inclusive of all services provided by family physicians in Canada, which generated the largest gaps across all service grouping scenarios. |
|||
Figure 2b. Base case workforce supply-demand gap, head counts, registered psychiatric nurses, nurse practitioners, occupational therapists, physiotherapists, and pharmacists, Canada, 2022-2034
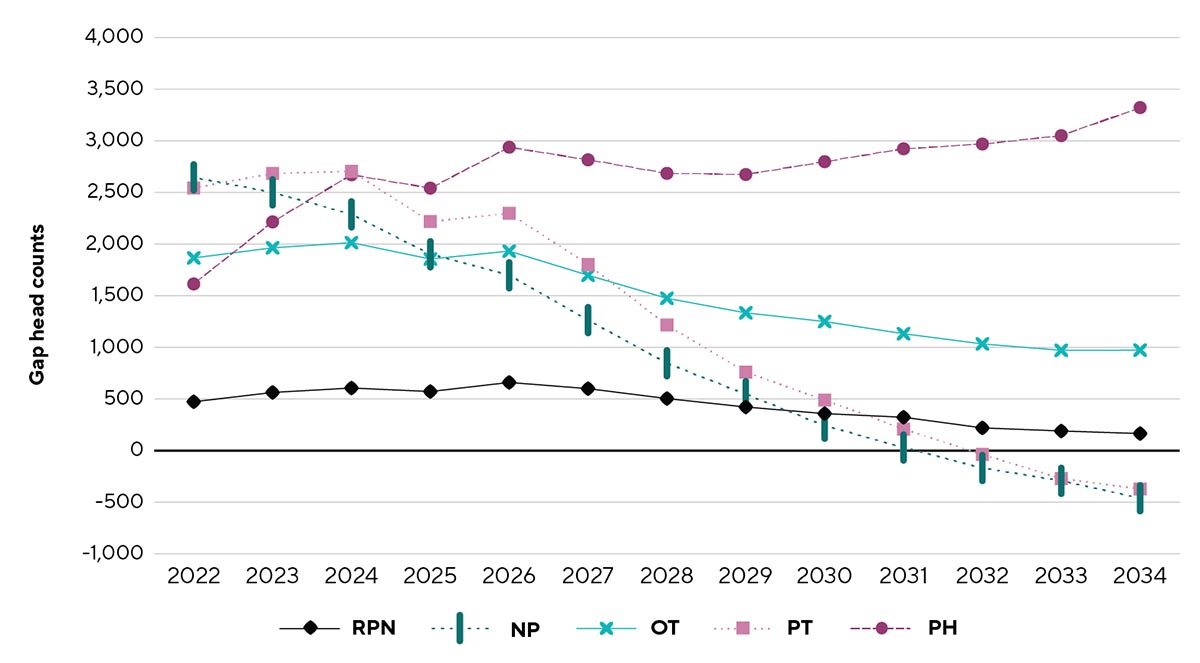
Figures 2a and 2b notes:
LPN: licensed practical nurse; RPN: registered psychiatric nurse; RN: registered nurse; NP: nurse practitioner; OT: occupational therapist; PT: physiotherapist; PH: pharmacist; FP: family physician. Source: Health Canada analysis using CIHI’s PRPT with adjustments and Health Canada’s pan-Canadian Health Workforce Projections Model. Family physician projection gaps are based on the scenario that is inclusive of all services provided by family physicians in Canada, which generated the largest gaps across all service grouping scenarios.
Figure 2b: Text description
Figure 2b presents a line graph illustrating the gap between supply and demand under the base case, in head counts, for registered psychiatric nurses, nurse practitioners, occupational therapists, physiotherapists and pharmacists in Canada from 2022 to 2034.
| Year | RPN | NP | OT | PT | PH |
|---|---|---|---|---|---|
| 2022 | 473 | 2,646 | 1,866 | 2,543 | 1,614 |
| 2023 | 563 | 2,501 | 1,964 | 2,684 | 2,215 |
| 2024 | 606 | 2,288 | 2,014 | 2,704 | 2,671 |
| 2025 | 572 | 1,901 | 1,855 | 2,218 | 2,542 |
| 2026 | 660 | 1,698 | 1,932 | 2,298 | 2,938 |
| 2027 | 600 | 1,264 | 1,698 | 1,802 | 2,816 |
| 2028 | 504 | 846 | 1,475 | 1,216 | 2,685 |
| 2029 | 422 | 547 | 1,334 | 760 | 2,674 |
| 2030 | 358 | 241 | 1,250 | 489 | 2,798 |
| 2031 | 323 | 30 | 1,132 | 208 | 2,923 |
| 2032 | 220 | -168 | 1,033 | -37 | 2,969 |
| 2033 | 190 | -293 | 971 | -271 | 3,050 |
| 2034 | 165 | -461 | 973 | -372 | 3,322 |
RPN: registered psychiatric nurse; NP: nurse practitioner; OT: occupational therapist; PT: physiotherapist; PH: pharmacist. Source: Health Canada analysis using Health Canada’s pan-Canadian Health Workforce Projections Model. |
|||||
The Study found there is a current need for almost 23,000 more family physicians (49% increase from current supply), 14,000 more licensed practical nurses (12% increase), 2,700 more nurse practitioners (35% increase), 28,000 more registered nurses (10% increase), 500 more registered psychiatric nurses (8% increase), 2,000 more occupational therapists (12% increase), 2,600 more physiotherapists (10% increase), and 1,700 more pharmacists (5% increase). See Table 3.
| Profession | LPN | RPN | RN | NP | OT | PT | PH | FP |
|---|---|---|---|---|---|---|---|---|
| Supply | 117,710 | 5,611 | 269,200 | 7,523 | 16,074 | 25,774 | 30,850 | 46,145 |
| Gap | 13,976 | 473 | 27,608 | 2,646 | 1,866 | 2,543 | 1,614 | 22,823 |
| Graduates | 6,295 | 336 | 8,992 | 550 | 873 | 770 | 1,217 | 1,362 |
LPN: licensed practical nurse; RPN: registered psychiatric nurse; RN: registered nurse; NP: nurse practitioner; OT: occupational therapist; PT: physiotherapist; PH: pharmacist; FP: family physician. Source: Health Canada analysis using CIHI’s PRPT with adjustments and Health Canada’s pan-Canadian Health Workforce Projections Model. Family physician projection gaps are based on the scenario that is inclusive of all services provided by family physicians in Canada, which generated the largest gaps across all service grouping scenarios. The number of graduates is based on the 2021-22 academic year. |
||||||||
Figures 3a and 3b show the gap as headcounts in urban geographic and in rural and remote areas, respectively, and over the projection period, highlighting the proportionally higher impact on rural or remote areas.
Figure 3a. Base case workforce supply-demand gap head counts per 1,000 workforce supply, urban areas, by profession, Canada, 2022, 2029 & 2034
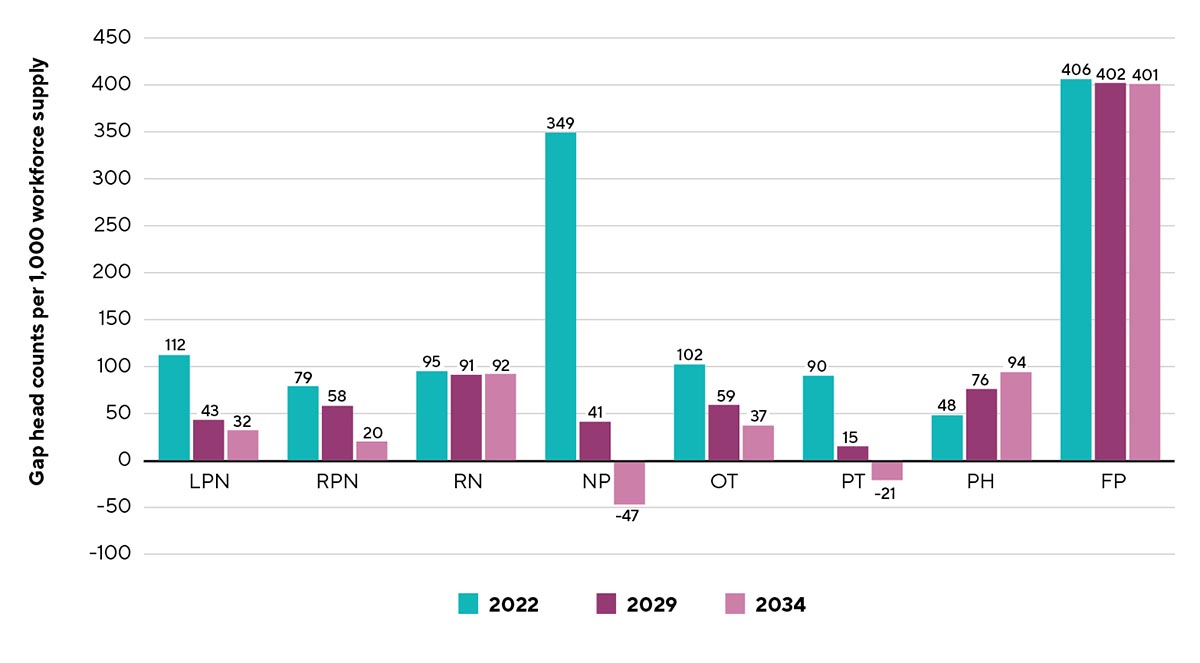
Figure 3a: Text description
Figure 3a presents a bar graph illustrating workforce supply-demand gap head counts per 1,000 workforce supply in urban areas under the base case, by profession, in Canada, for 2022, 2029 and 2034.
| Urban areas | LPN | RPN | RN | NP | OT | PT | PH | FP |
|---|---|---|---|---|---|---|---|---|
| 2022 | 112 | 79 | 95 | 349 | 102 | 90 | 48 | 406 |
| 2029 | 43 | 58 | 91 | 41 | 59 | 15 | 76 | 402 |
| 2034 | 32 | 20 | 92 | -47 | 37 | -21 | 94 | 401 |
Figure 3b. Base case workforce supply-demand gap head counts per 1,000 workforce supply, rural or remote areas, by profession, Canada, 2022, 2029 & 2034
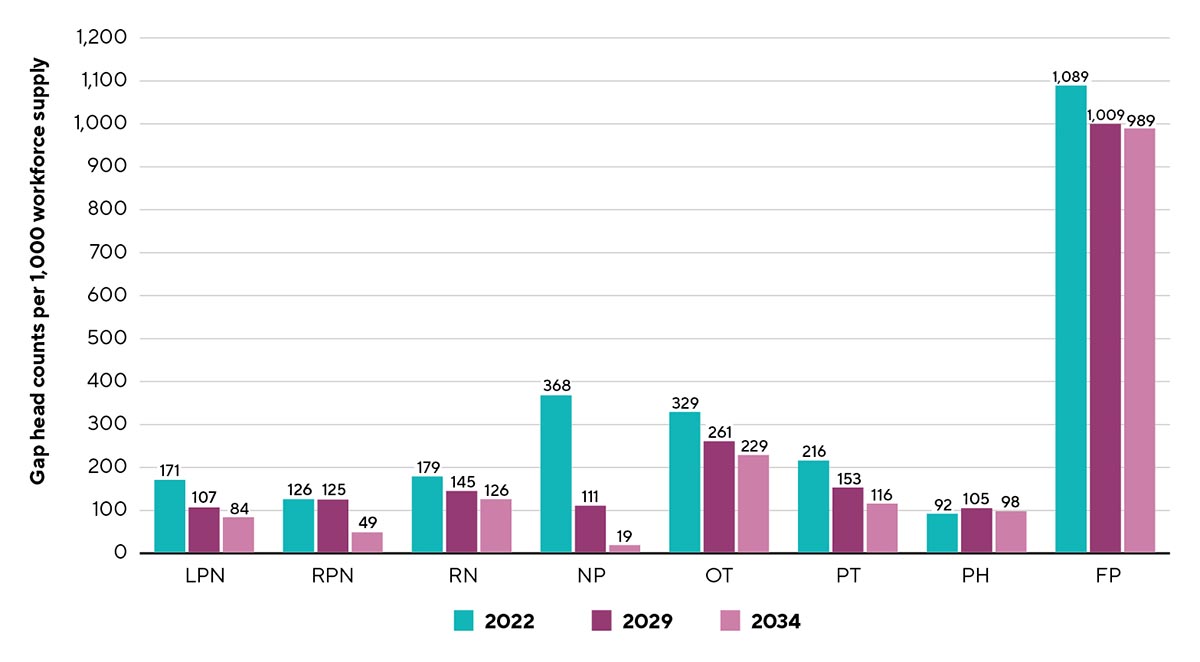
Figures 3a and 3b notes:
LPN: licensed practical nurse; RPN: registered psychiatric nurse; RN: registered nurse; NP: nurse practitioner; OT: occupational therapist; PT: physiotherapist; PH: pharmacist; FP: family physician. The FP gap results reflect the all services scenario of the base case analysis.
Figure 3b: Text description
Figure 3b presents a bar graph illustrating workforce supply-demand gap head counts per 1,000 workforce supply in rural and remote areas under the base case, by profession, in Canada, for 2022, 2029 and 2034.
| Rural and remote areas | LPN | RPN | RN | NP | OT | PT | PH | FP |
|---|---|---|---|---|---|---|---|---|
| 2022 | 171 | 126 | 179 | 368 | 329 | 216 | 92 | 1,089 |
| 2029 | 107 | 125 | 145 | 111 | 261 | 153 | 105 | 1,000 |
| 2034 | 84 | 49 | 126 | 19 | 229 | 116 | 98 | 989 |
Nurse practitioners and physiotherapists are the only in-scope professions who are projected to have additional capacity by the end of the projection period. The increase in NP supply is in part driven by the increase in educational and training seats that have been added across the country in recent years and those which are planned for future years. These additional seats will lead to a substantial growth in supply of NPs in certain jurisdictions. For physiotherapists, the projections model uses historical inflows which have recently been higher than outflows based on the workforce data from CIHI, resulting in positive net new workforce supply values that eventually lead to supply exceeding demand starting in 2032.
The data used in the analyses are limited in terms of timeliness and accuracy. In many circumstances, the analysis relied on imperfect data as proxies for missing information. Further, although efforts were made to apply assumptions to the projections based on evidence, there were times when data were not available or reliable. Therefore, assumptions could be made on reasonableness based on consultation with experts.
Additional scenario analyses, exploring the potential future circumstances that may impact projected workforce supply-demand gaps, show that increasing population size and disease prevalence would substantially increase the projected gaps across all professions. Further, expanding the potential for nurse practitioners to increase primary care attachment could also increase demand and the gap for that profession, while reducing demand and the gap for family physicians. Lastly, early retirement in the professions would significantly reduce supply, thus widening the workforce supply-demand gaps over time.
Projections can only account for what we know today. There are a multitude of factors that can play a significant role in health workforce supply and demand into the future. Examples include policies that optimize scope of practice and that reduce financial barriers to accessing certain types of care provided by different health professionals, among others. Projections for the purpose of health workforce planning should not be a one-time process. Continual refinement and data updates to these models will improve their validity, reliability and usefulness.
Given the limitations associated with the workforce supply and demand projections, including data and modelling constraints and the high level of uncertainty for the future, the specific numbers reported in the results should be interpreted and used with caution. Nevertheless, the overall direction of the results provides a strong message regarding the current and future challenges in meeting population health needs with a sufficient domestic supply. Across most occupations, the current state and projection results show substantial supply-demand gaps now and over the next 10 years.
A more fulsome analysis on meeting primary health care needs could better establish demand for health care providers working in interprofessional primary care teams. These teams could include health professionals who provide comprehensive primary care in the areas of mental health, physical rehabilitation, medication management, as well as other types of primary care, all of which can be provided by the health professions within scope of the Study, as well as several others.
These results must be considered within the context of health professional work requirements, patterns of work and demographics, and regional differences (urban versus rural and remote). Health professions education and workforce planners must compare these results to their data at the PT, regional and local levels.
Rural and remote consideration
All Study parameters are more concerning in rural and remote areas. The Study was unable to determine how many health professionals come from rural and remote communities or trained in these communities. Proportionally, the needs of rural and remote communities are higher, the supply is lower, and the gaps will increase over time. The workforce projections modelling used for the Study did not consider the need for locum (in other words, temporary) and replacement workers which has an even bigger impact on rural and remote communities. In consultations, rural and remote health care providers described how their health workforce issues were more similar to others in rural and remote areas across the country than to urban issues within their own jurisdiction. Working collaboratively as a Canadian collective or network, particularly for rural and remote areas, was deemed beneficial.
Several innovations across the country are underway that have demonstrated positive results. The most enduring efforts involve training health professionals in rural and remote areas, where they are supported by rural preceptors and reside in the communities in which they learn and provide care. These initiatives would require significant spread to all rural and remote regions for maximal impact in increasing the supply in these areas.
Physicians and family physicians
The shortage of physicians in Canada is not surprising as Canada has been underproducing medical graduates for decades. According to the 2023 OECD Health Report, Canada has 2.8 practicing physicians per 1,000 population with the OECD average at 3.7 per 1,000 population. Norway has 5.4 per 1,000 population. With the 2023 OECD average number of new graduates at 14.2 per 100,000 population, Canada produces 7.5 per 100,000 with only Japan, Korea and Israel lagging behind. Denmark produces 22 new graduates per 100,000 per year.Footnote 4
Several recent publications have highlighted the extent of the deficit of physicians in the health workforce. For the physician workforce in the United States, the Association of American Medical Colleges projected a shortage of 86,000 physicians and, if no increases are made in the number of residency positions, the United States is projected to have a deficit of over 124,000 physicians by 2034.Footnote 5 In the UK, a 2018 report from the Royal College of Physicians estimated that the total annual intake of medical students needed to double to meet population needs in 2030.Footnote 6
Consideration must also be given for the fact that physician hours worked has shifted over time with a recent study showing that the 3-year moving average of physician weekly hours worked dropped 13.5%, from 52.7 hours per week in 1988 to 45.6 hours per week in 2019.Footnote 7
Family physicians are key to the provision of primary care in Canada. In 2024, the CD Howe Institute reported that Canada currently has a deficit of 13,845 family physicians.Footnote 8 Although historically the vast majority of family physicians provided comprehensive “cradle to grave” care, this approach to care has shifted over time. In 2022, the University of Alberta found that only 38.8% of surveyed family medicine residents were intending to practise clinic-based longitudinal care and take on a patient panel as one indication of providing continuity of care. In the same report, 72.6% of residents reported that prior to entering residency they had anticipated that they would take on a patient panel.Footnote 9 In British Columbia, there is evidence that although the number of family physicians is increasing, the increase in care provision is seen mainly in emergency departments, hospital care, mental health, substance use, and other focused areas, not in rostered general practice.Footnote 10 There is evidence that this trend is similar across the country.
When determining how many students to admit to medical school, consideration must be given to how many will then enter a family physicians residency (for example, based on number and ratio of positions available). Appropriate education and workforce planning can only take place with the understanding that some of the new family physicians will choose to provide comprehensive care and take on a roster or panel of patients while others will be providing care in emergency departments, in hospitals, in palliative care, and other health care settings.
Nurses (LPN, RPN and RN)
Nursing is the largest group of regulated health professionals in Canada,Footnote 11Footnote 12 and since the nursing profession is fundamental to a functioning health care system, educating a strong nursing workforce must be a priority.Footnote 13 All four nursing categories need to increase their education seats to meet current and future population needs. Although RPN programs currently only exist in the western provinces (specifically, BC, AB, SK and MB), they are also being licensed in the territories and may soon be licensed in the Atlantic provinces.Footnote 14 Given this increase in jurisdictions licensing RPNs, additional provinces and territories may wish to offer RPN education programs as Study data suggest that they will be in even greater need in the future. Additionally, other jurisdictions should consider establishing LPN training programs as well given that this is a key nursing role with a lower barrier entry to the nursing profession (for example, two years of education at college level). Retention is a significant issue in the nursing profession. Nursing education programs face challenges finding faculty and clinical resources including preceptors and placements, and healthcare settings are strained to accommodate students, resulting in attrition from nursing education programs and a failure to retain nurses once they are licensed and registered to practise. Solutions must be aimed at the work environment in order to retain nurses in the profession.Footnote 15
Nurse practitioners
Although there has been a historic underutilization of NPs, they are progressively recognized as having a key role in primary care.Footnote 16Footnote 17 The Study data reveals that, as their training seats have increased and will continue to increase in the near future, and based on current demand, supply could meet demand by 2031. This may be an opportunity for health workforce planners to consider increasing the role of NPs, to help meet primary care needs in their jurisdiction. This could have a significant impact on reducing the need for other primary care providers where a significant gap exists, such as with family physicians.
Occupational therapists, physiotherapists and pharmacists
These three health professions provide unique and essential care for Canadian populations. They all contribute to care in a wide variety of settings from hospital, long-term care, palliative care, specialty care and primary care. Their training models have changed over time with a transition to master's programs for occupational therapists and physiotherapists and towards a mandatory Doctor of Pharmacy program for pharmacists. The Study data indicate that an important gap exists between current supply and demand. The number of training seats in these health professions over the last five years have been static (less than 1 % increase) and that the projected increase in the next 10 years is between 1-2%. This planned capacity change will not address the current and predicted gap.
Primary care health professionals
Although family physicians have historically been the primary care providers in most parts of Canada, this is changing across the country. Nurse practitioners are taking on an increasingly important role as primary care providers and the current increase in training seats for NPs in many provinces should help alleviate the current deficit in family physicians.
Depending on the model of primary health care team established in a jurisdiction, other health professionals within scope of the Study such as nurses, physiotherapists, occupational therapists, and pharmacists, and others such as physician assistants, midwives and paramedics can be important contributors to primary care. If all health professionals are working at the top of their scope of practice within a primary care team, this could significantly increase the potential panel size for a family physician while also reducing their administrative burden. If compensation models are addressed for these health professionals, this type of comprehensive team-based primary care environment would be a very attractive career option.
Challenges and barriers
Many challenges and barriers exist in the provision of education for all in-scope health professions and include, but are not limited to, the need for an increased number of training seats in an environment with a limited number of teachers, faculty members and preceptors; a scarcity of clinical placements; lack of investment in simulated learning opportunities; difficulty accessing the required number of patients; lack of remuneration or incentives for preceptors; and insufficient administrative resources and funding. Current health workforce realities can account for some of the significant challenges in the provision of education for the health professions studied given the difficulty accommodating learners as supernumeraries when healthcare delivery is so strained.
Occupational therapy and physiotherapy, in particular, identified educational accreditation requirements for excessive numbers of patient contact hours as a significant barrier to their ability to accept more students.
Tuition and program costs were highlighted as a barrier for students and may have a negative effect on a program’s ability to enroll students of diverse backgrounds and from marginalized populations. This was an even more important factor for rural and remote programs where students may have to pay for housing in more than one location at one time, and cover travel costs as well.
Innovations
Innovations in health professions education are underway across the country. The Study provides a sampling of the innovation that is ongoing with examples from all professions included in the Study and from each province and territory.
Innovative opportunities include targeted admission support for students who are currently underrepresented; on-line, virtual or distance education to accommodate students who are from various geographic locations; and programs or rotations offered in rural and remote areas supervised by local health professionals.
Curricular design flexibility is apparent with accelerated pathways, bridging and “learn as you earn” programs as well as direct entry primary care medical education programs. Education in interprofessional and First Nation, Inuit and Métis community settings are critical innovations for more integrated team-based care.
The opportunity exists for many of the innovations cited in the full Study report to be spread and scaled to other jurisdictions, as appropriate, given the local context. If such spreading in innovation were to occur, significant improvement in care would be noted overall and most significantly for rural, remote and Indigenous populations.
Interprofessional health professions education and workforce planning
Integrated and collaborative policies across education and health service delivery can coordinate optimal health workforce outcomes.Footnote 18 This interprofessional form of planning is in contrast to the usual siloed health profession-specific approaches. While more complex at the outset, many countries are moving in this direction. The United Kingdom, Brazil, Australia, and Norway have legislated mergers between previously siloed sectors, such as education, accreditation, health and social service delivery systems and government.Footnote 19
One example of work undertaken in Canada, Team Primary Care, is a multi-partnered initiative recently funded by Economic and Social Development Canada to enhance the capacity of interprofessional, comprehensive primary care through improved training, team supports, and planning tools for employers and planners.Footnote 20
Reflections
The Study’s request for information on the education and training capacity has reinforced the need for a standardized approach to data collection for health professions education across Canada. Except for physicians, is not possible to follow a health professional from training through practice and retirement. This is a significant limitation in health workforce planning as jurisdictions are unable to track graduates into and out of the workforce, or movement between categories of professionals (such as, LPN to RN or RN to NP) or between different professions altogether (such as, physiotherapists or occupational therapists to medicine).
As jurisdictions have separate ministries of education and health, collaborative data sharing and health workforce planning are not inherently part of the departmental structures. This must be addressed for health professions education and training to respond to the health care needs within the jurisdiction.
Future work in improving data quality, integrity, comprehensiveness and timeliness is important to improve the robustness of the results, as are continual refreshes on the modelling with these new data. These analyses should be considered a starting point in better understanding some of the potential challenges and opportunities in connecting education and training capacity, and workforce supply and demand today, and into the future.
Given the complexity of issues related to the health system and its workforce, there is no one policy lever that will address all desired outcomes. Health workforce planning should function as an adaptive learning system that is evidence informed, integrated and interactive.Footnote 21 This endeavour can only be successful if there is a regular influx of timely, good quality data.
Recommendations
Education, training and health workforce data
A minimum data standard on health professions students and their education programs should be created and required for all health profession programs to complete and report on.
Data on health professions students and their education programs should be available to those who undertake health workforce planning.
Health professions students should have a unique identifier that will not change through their entire professional career to facilitate monitoring of location and practice patterns for health workforce planning purposes.
For the Indigenous health workforce, collaborative efforts should be made to co-develop data collection processes, forecast workforce needs, and create culturally appropriate health programs and services. Regular monitoring and reporting on the progress of Indigenous health workforce recruitment, retention, and educational outcomes are crucial for accountability.
Health professions education and training planning
Significant increases in education and training seats are required to meet the current and future demand for nurses, occupational therapists, physiotherapists, pharmacists and family physicians in Canada. Specific gaps and needs must be determined by PT health profession education and health workforce planners.
Health professions education planning should be undertaken with an interprofessional approach involving, at a minimum, PT ministries of health, PT ministries of education, health professions education leaders, health care institutions, and community members.
In collaboration with First Nations, Métis and Inuit community leaders and organizations, educational pathways that consider the unique lived experiences of Indigenous learners and address barriers such as access to education, cultural safety, anti-Indigenous racism, language challenges, and recruitment and retention criteria must be developed to increase the recruitment of Indigenous students into health professions. Additionally, enhanced culturally relevant student and professional supports should be provided.
Health professional education and training should be structured from a perspective of required competencies for primary care.
Health workforce projection modelling
An FPT community of practice for health workforce modellers in Canada should be developed to enable the application of new technical approaches to modelling and the use of different data and assumptions that would generally improve health workforce planning at various levels.
Integrated supply and demand projection models for interprofessional primary care teams should be created based on population health needs to improve decision makers’ ability to develop interdisciplinary care teams that optimize the health workforce.
Rural and remote education
The minimum data standard on health profession students should include information regarding student location at the time of application, during education and practice location.
Health profession students from rural and remote communities should be supported to enroll in programs with training in rural and remote communities by local preceptors and supported by the communities in which they train. Should they require advanced training away from their communities, opportunities and incentives should be in place to return to their community.
The additional educational support required for rural and remote education programs and their teachers and preceptors should be considered in the financing of rural and remote education programs.
A rural and remote health professional education and training network across PTs should be established to enable collective sharing of innovative practices and solutions.
Sustainable resourcing mechanisms that support the long-term implementation of Indigenous-led recruitment and retention strategies for roles based within Indigenous communities and nations, that contribute to health workforce education and training, must be established.
Employer role
Health care employers should be ensuring the successful transition of new graduates and provide support and mentoring as they enter into practice. Employers should be attentive to the need for a positive work environment and actively address retention efforts.
Health professions role
Accreditation and regulation of health professions education must adapt as quickly as necessary to align changes to the education and training of health professionals to respond to societal needs.
Health professions education leaders need to work collaboratively to accelerate interprofessional educational transformation aligned with primary care competencies. Creating a new structure to break down the silos that currently exist would be beneficial.
Health professional associations should encourage their members to engage in the education of the next generation of health professionals as clinical faculty and preceptors and support their professional development as teachers.
Ongoing study
Ongoing work to access and create health professions education and training capacity data for cyclical reporting should be undertaken to help inform health workforce projections at a pan-Canadian level.
Data on all health professions (and other specialties) should be collected and considered in health workforce planning. Record level standardized data, with timely collection, need to be updated on a regular basis to produce reliable forecasting estimates that can be tracked and adjusted over time.
Engagement is required with First Nations, Métis and Inuit organizations across the country to determine the best ways forward to identify and build on Indigenous-led solutions to grow the Indigenous health workforce. Building relationships and enhancing resources are key strategies for amplifying opportunities and incentivizing accessible education and training, while formal partnerships with Indigenous health authorities and organizations are essential to sustain recruitment and retention efforts.
Future work should consider the needs of other equity deserving groups and marginalized populations with a focus on educating future health professionals in culturally safe care for people in Canada.
Future considerations
This Study is the first national initiative of its kind to collect information on the education and training of select health professionals, and to provide estimated supply-demand projections for multiple health professions. This information will be critical to support considerations on next steps to address the supply challenges within the health workforce. This work builds on current efforts being made across Canada to develop appropriate health workforce models that can assess the gap between the supply and demand of health professionals. Policy makers across the country are also working on other important areas such as increased scope of practice, moving towards more team-based primary care models, and supporting qualified internationally trained health care professionals to practice in Canada.
Canada clearly has urgent work to do to address the current and future gaps in the number of health professionals studied. While investing in this enhanced training capacity, innovations highlighted in the Study can be scaled and spread to accelerate positive change. Regular review of projections must be undertaken using up to date information from reliable sources. A commitment to establishing robust data requirements, and collaboration between health profession education and workforce leaders, are key to supporting the complex adaptive system required to succeed in providing the health workforce Canada needs. We have a strong workforce; we must now find a way to better leverage those strengths and innovate at the same time.
By addressing the recommendations, health ministries, in concert with regional health and educational institutions, can contribute to building a more equitable and culturally informed education and training experience to broaden the health workforce in Canada. Collective and coordinated actions are crucial to increase Indigenous health human resources, in pursuit of advancing reconciliation and improving health outcomes for Indigenous Peoples from coast to coast to coast. Effective collaboration and sustained investment in Indigenous health education through to health professions programs supported by intentional decolonial workforce development efforts are essential steps towards achieving these goals.
An ideal future state for health professions education and workforce planning is one where a minimal data standard exists that allows knowledge of the individual as a trainee and a worker along their career trajectory. Data would be regularly inputted from appropriate sources to allow cyclical adjustments to databases to help adapt projections and implement any required changes in education seats and other parameters. Second, an interprofessional health profession education and workforce planning collaborative council is established including ministries of health and education, Indigenous leaders, employers, regulators, accreditors, educators, learners and communities to collectively address the health and health care needs of Canadian populations. Third, a transformative learning health workforce education system is created where timely adaptations of policy decisions are based on a regular stream of robust data to inform and enable adjustment of assumptions for best modelling and predictions is possible.
With collaboration and coordination amongst all key stakeholders, Canada can reach the goal of caring for Canadians by educating Canada’s future health workforce.
References
- Footnote 1
-
Truth and Reconciliation Commission of Canada. Truth and Reconciliation Commission of Canada: Calls to Action. Manitoba, Canada; 2015 [cited 22 August 2024]. Available from: https://publications.gc.ca/collections/collection_2015/trc/IR4-8-2015-eng.pdf
- Footnote 2
-
United Nations. United Nations Declaration on the Rights of Indigenous Peoples. 2007 [cited 22 August 2024]. Available from: https://www.un.org/development/desa/indigenouspeoples/wp-content/uploads/sites/19/2018/11/UNDRIP_E_web.pdf
- Footnote 3
-
Van Mulligen L. Addressing Student Attrition in Nursing Education Programs. BU Journal of Graduate Studies in Education. 2022; 14(3): 4-8 [cited 16 July 2024]. Available from: https://files.eric.ed.gov/fulltext/EJ1350841.pdf
- Footnote 4
-
OECD Health at a Glance 2023: OECD Indicators, OECD Publishing, Paris; 2023. https://doi.org/10.1787/7a7afb35-en
- Footnote 5
-
GlobalData Plc. The Complexities of Physician Supply and Demand: Projections From 2021 to 2036. Washington, DC: AAMC; 2024 [cited 10 July 2024]. Available from: https://www.aamc.org/media/75236/download?attachment
- Footnote 6
-
Britnell, M. Human: Solving the global workforce crisis in healthcare. Oxford, Oxford Academic; 2019.
- Footnote 7
-
Kralj B, Islam R, Sweetman A. Long-term trends in the work hours of physicians in Canada. CMAJ 2024; 196(11):E369-E376. https://doi.org/10.1503/cmaj.231166
- Footnote 8
-
Zhang T. The Doctor Dilemma: Improving Primary Care Access in Canada. CD Howe Institute; Commentary 660. http://dx.doi.org/10.2139/ssrn.4839693
- Footnote 9
-
Horvey S. RE: Changes over time in patient visits and continuity of care among graduating cohorts of family physicians in 4 Canadian provinces. CMAJ. 2024, March 13 [cited 8 October, 2024]. Available from: https://www.cmaj.ca/content/re-changes-over-time-patient-visits-and-continuity-care-among-graduating-cohorts-family
- Footnote 10
-
Lavergne MR, Rudoler D, Peterson S, Stock D, Taylor C, Wilton AS, et. al. Declining comprehensiveness of services delivered by Canadian family physicians is not driven by early-career physicians. Ann Fam Med. 2023;21(2):151-156. https://doi.org/10.1370/afm.2945
- Footnote 11
-
Canadian Nurses Association. Nursing Statistics. 2024 [cited 8 July 2024]. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-statistics
- Footnote 12
-
Ahmed, HEB, Bourgeault IL. Sustaining Nursing in Canada. Ottawa, Canadian Federation of Nursing Union; 2022 [cited 8 July 2024]. Available from: https://nursesunions.ca/wp-content/uploads/2022/11/CHWN-CFNU-Report_-Sustaining-Nursing-in-Canada2022_web.pdf
- Footnote 13
-
Canadian Association of Schools of Nursing (CASN). CASN Strategic Plan 2023 – 2028. No date [cited 8 July 2024]. Available from: https://www.casn.ca/about-casn/casn-strategic-plan-2023-2028/
- Footnote 14
-
Nova Scotia College of Nursing. Maritime-wide Registered Psychiatric Nurse (RPN) Feasibility Study Report Now Available [News Release]. 2023 [cited 8 July 2024]. Available from: https://www.nscn.ca/explore-nscn/news-and-media/news/2023/maritime-wide-registered-psychiatric-nurse-rpn-feasibility-study-report-now-available
- Footnote 15
-
Health Canada. Introduction: Nursing Retention Toolkit. 2024 [cited 18 June 2024]. Available from: https://www.canada.ca/en/health-canada/services/health-care-system/health-human-resources/nursing-retention-toolkit-improving-working-lives-nurses/introduction.html
- Footnote 16
-
Almost, J. Regulated nursing in Canada: The landscape in 2021. Canadian Nurses Association; 2021 [cited 10 July 2024]. Available from: https://hl-prod-ca-oc-download.s3-ca-central-1.amazonaws.com/CNA/2f975e7e-4a40-45ca-863c-5ebf0a138d5e/UploadedImages/documents/Regulated-Nursing-in-Canada_e_Copy.pdf
- Footnote 17
-
Canadian Federal of Nurses Union. Fulfilling Nurse Practitioners’ Untapped Potential in Canada’s Health Care System: Results from the CFNU Pan-Canadian Nurse Practitioner Retention & Recruitment Study; 2018 [cited 8 July 2024]. Available from: https://nursesunions.ca/wp-content/uploads/2018/06/CFNU_UntappedPotential-Final-EN.pdf
- Footnote 18
-
Tomblin Murphy G, Gilbert JH, Rigby J. Integrating interprofessional education with needs-based health workforce planning to strengthen health systems. J Interprof Care. 2019;33(4):343-346. https://pubmed.ncbi.nlm.nih.gov/31385731/
- Footnote 19
-
Canadian Academy of Health Sciences. Canada’s Health Workforce: Pathways Forward. An Assessment by the Canadian Academy of Health Sciences. 2023 [cited 7 October 2024]. Available from : https://cahs-acss.ca/wp-content/uploads/2023/04/CAHS-Health-Workforce-Pathways-Forward-EN_Final_Apr-4.pdf
- Footnote 20
-
Team Primary Care. About Team Primary Care. No date [cited 10 July 2024]. Available from: https://www.teamprimarycare.ca/
- Footnote 21
-
Bourgeault IL, Chamberland-Rowe C, Simkin S. Co-developing an integrated primary care workforce planning approach at a regional level: overarching framework and guiding principles. Hum Resour Health. 2021; 19(87). doi: 10.1186/s12960-021-00578-z
Page details
- Date modified:
